What becomes of the broken hearted? Blueprint of a donor-free world using custom heart technologies
Advances in 3D-printing technology have the potential to lower the cost and increase the availability of organ transplants.
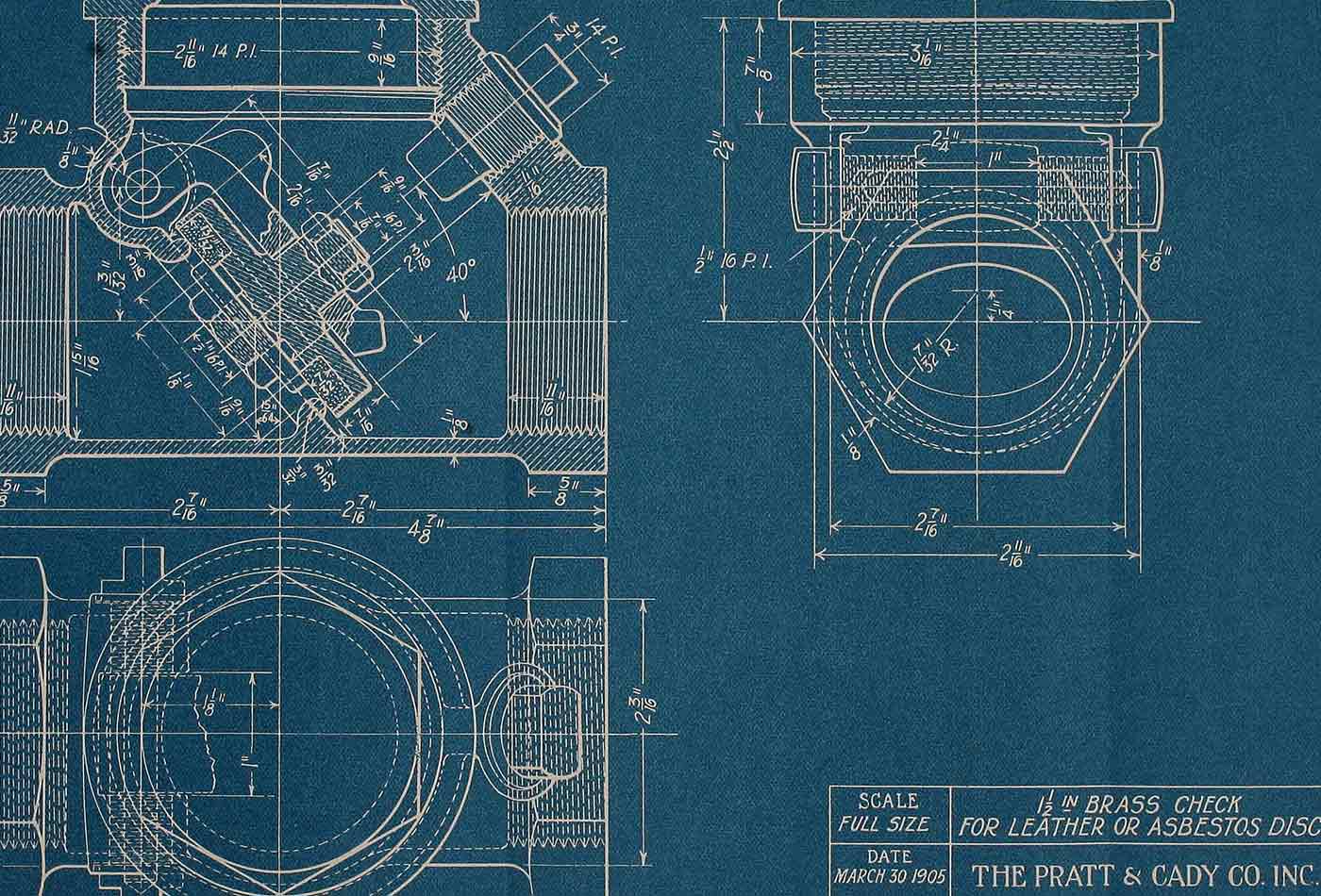 Blueprint reading, a practical manual of instruction (source: Internet Archive on Flickr)
Blueprint reading, a practical manual of instruction (source: Internet Archive on Flickr)
Imagine feeling like you ran a marathon when you’re actually just getting off the couch. Imagine the extreme anxiety you might experience from living with bouts of dizziness, chest pain, and accelerated heartbeat until a doctor explains to you that these symptoms are not “nothing”, and that in fact, you have cardiomyopathy. This condition could lead to heart failure and eventually a heart transplant, but this desperately needed organ may not be available in time.
Organ transplants are in high demand in the United States. The heart is the third most requested organ, with 4,000 candidates on the waitlist and over 2,000 heart transplant surgeries performed in 2017.
Heart transplantation is an exorbitantly expensive procedure (Table 1-1) with a myriad of potential complications. Rejection is an unsolved problem and has remained for all these years a major risk of all organ transplants.
| Per heart transplant | Cost (US dollars) |
|---|---|
| 30 days pre-transplant | $43,300 |
| Procurement | $102,100 |
| Hospital admission | $887,400 |
| Physician during transplant admission | $92,300 |
| 180 days post-transplant | $222,800 |
| Immuno-suppressants & other | $34,500 |
| Total | $1,382,400 |
If a heart substitute could be developed, capable of emulating a human heart, this would address a critical need for patients in these dire straits.
Moreover, a lab-grown heart might be free of rejection issues if a patient’s own cells are used, thus economizing the total cost of heart transplant from $1,382,400 to $1,245,800 by eliminating procurement, the surgery to remove the organ from the donor, and immuno-suppressants (Table 1-1).
This $136,600 per transplant saving translates to approximately $300 million from the 2,000 surgeries performed in 2017. Given the 4,000 patients on the waitlist, a rough estimate of the market size of a human heart substitute could reach nearly $1 billion per year for the custom heart industry in the US.
Scientists have been working to address the gap in the shortage of tissue transplants. New opportunities have opened in the past decades as many of the technological limitations have been overcome by important innovations in stem cell biology.
Stem cells are highly pluripotent, with the ability to differentiate into any cell type in the body. Breakthroughs in induced pluripotent stem cells (iPSC) allow for reprograming somatic cells and have made it possible to obtain pluripotent, embryonic-like stem cells without embryos. Cells derived from iPSCs can serve as building blocks for tissues, turning the idea of growing organs outside of the body from science fiction to reality.
While we are able to grow pieces of heart muscle iPSCs to patch small, damaged areas (like Nenad Bursac’s group at Duke University did)—an achievement in itself—there are many obstacles to overcome when building a replica of the human heart due to its complex structure and composition.
Nevertheless, building something that is functionally identical to a heart may be possible. Many interesting approaches are currently being explored to produce adequate, artificial replacements for this most critical organ.
Recycling an Unusable Heart
Time is critical in organ transplantation. When a donor heart becomes available, it can only be preserved for a short time for transplantation. As a result, 20% of donated hearts go to waste because they cannot be transplanted to a recipient in time.
What can we do with these “unusable” hearts? Harald Ott’s group at Harvard Medical School and Massachusetts General Hospital found a way to give them new life.
Using a detergent solution, the researchers first strip the cells, DNA and lipids from the heart, leaving an intact, complex acellular cardiac extracellular matrix (ECM) scaffold.
This cell-free scaffold is a mesh that holds the heart together and contains blood vessels that can transport oxygen, nutrients, and waste. Next, they re-seed the ECM with new cardiomyocytes derived from iPSCs to form the muscular wall of the heart.
The re-cellularized ECM is incubated in a bioreactor which could provide all nutrients and mechanical stimulations needed for tissue development. After two weeks, the ECM is covered with layers of cardiomyocytes and exhibits functional contraction upon electrical stimulation.
Several challenges remain to be addressed in this approach, including ensuring that the right number of cells are in the right combination for proper heart function, as well as engineering a bioreactor that better mimics the human body. Despite these obstacles, this approach has served as a convincing proof-of-concept that functional hearts can be re-grown in labs on existing cardiac ECMs
Building a Vegetarian Heart
As an alternative to using ECMs from animal sources, a multi-institutional collaboration among Worcester Polytechnic Institute, the University of Wisconsin-Madison, and Arkansas State University-Jonesboro seeks to develop plant-based ECM scaffolds.
This idea is far from intuitive, given the vast differences between animals and plants. However, plant vascular structures follow many of the similar physiological laws as the cardiovascular systems of animals. More importantly, an ECM from plants is mainly composed of biocompatible materials, making it an ideal candidate for a lab-grown organ.
In a procedure analogous to the one just described, scientists first wash away the cellular material from a spinach leaf to obtain an acellular ECM with functional veins. The spinach ECM is then coated with human endothelial cells on the leaf vasculature and seeded with human cardiomyocytes.
After a few days, the cells attach to the spinach ECM and contract in the same way as cells grown in a tissue culture. This demonstrates the possibility of culturing human cells on a plant scaffold. However, how well plant veins can sustain human tissue and the immune response against the plant scaffold still requires further investigation.
Exploiting a Pig’s Heart
While the heart is a delicate and complicated machine, it is hardly unique to humans. Could we substitute human heart with a heart from an animal? This process is known as xenotransplantation.
In the mid-20th century, severe immune responses made all xenotransplantation between nonhuman primates and humans fatal. However, in recent years, with better understanding of the human immune system, xenotransplantation has gradually regained attention and consideration.
Among all of the possible animal donors, the pig is considered to be the best candidate, as it is widely accessible, genetically similar to humans, and has organs of approximately the same size.
The creation of a genetically engineered pig lacking the gal gene, a main trigger of human immune reaction, has significantly extended the survival time of baboons receiving these porcine organ transplants.
Muhammad Mohiuddin’s group at the National Heart, Lung, and Blood Institute, took a step further with the gal knockout pigs. By inserting two human proteins that prevent host cell damage and blood coagulation into the gal-free pig genome, his group was able to keep a porcine heart alive in a baboon for over two years.
Delayed rejection ultimately happened and led to the death of the baboon, but modifying pig genes, altering the types and expression levels of human genes in pigs, and optimizing anti-rejection drugs may lead to a viable system of xenotransplantation.
In addition to rejection complications, viral infection is another concern for xenotransplantation. Genes from ancient infections from porcine endogenous retroviruses (PERV) are scattered throughout a pig’s genome.
Although it is not clear whether PERVs could actually produce viral particles capable of infecting humans, the presence of those viral remnants still generates concerns among the scientific community and casts a shadow on the use of xenotransplantation.
To overcome this problem, eGenesis, a Boston-based startup, has devoted its expertise in genome editing to make PERV-free pigs. Founded in 2015 by geneticists Luhan Yang and George Church from Harvard Medical School, the company’s mission is to use genome editing to make safe human tissues and organs for transplant.
Still at an early stage, the company announced in March 2017 a $38 million series A financing led by Biomatics Capital and ARCH Venture Partners. Their recent study using CRISPR-Cas9 facilitated multiplex genome editing and successfully removed all PERV genes from the pig genome, producing the first batch of PERV-free piglets. This groundbreaking progress is an important step toward eliminating potential viral infections and to making xenotransplantation safer.
Crafting a Chimera Heart
If a porcine heart for transplant is not readily available, perhaps growing a human heart inside a pig (known as a chimera) may be a more straightforward approach.
Along those lines, Juan Carlos Izpisua Belmonte’s group from the Salk Institute has successfully developed a rat-mouse chimera with a rat-cell-enriched pancreas. They have done this by injecting rat pluripotent cells into a mouse embryo lacking a critical gene for pancreas development.
This success led researchers to conduct a pioneering experiment in which they injected human pluripotent cells into pig blastocysts which were grown into viable human-pig chimeric embryos. However, chimeric embryos exhibited low human cell content and slow growth rates, due to the significant evolutionary distance between humans and pigs.
Nevertheless, this was the first successful example of introducing human stem cells into large animals and was a significant step toward growing transplantable human tissues/organs in host animals.
Human-animal chimera research is a heavily debated issue, with the public expressing concerns that such research could blur the border between humans and other species.
The National Institutes of Health (NIH) also prohibit several approaches in creating human-animal chimeras, but they are now considering revising their policy in order to better guide the rapid progress of the field.
Resuming 3D Printing
Earlier 3D bioprinting focused on generating molds for cells to attach. Although this approach cannot produce solid organs, the possibility of “printing” an organ remains an attractive direction for researchers to pursue.
Creating a scaffold with a vascular system is one of the biggest challenges in tissue printing. Anthony Atala’s group from the Wake Forest Institute for Regenerative Medicine recently reported a 3D printing system that can print layers of cells with biodegradable plastic micro-channels that mimic vascular systems.
Prellis Biologics, a San Francisco-based startup, is working on printing blood vessels based on real human vascular data. Its proprietary 3D laser-based printing technique adapts information from a microscope, with the projected laser polymerizing bio-substrates at very high resolution. In combination with computer-aided design, it’s able to build a precise scaffold system to support the cells and tissues.
The company recently received a $1.8 million seed investment and a total of $1.92 million led by True Ventures. The company’s early goal is to print a human organoid, a miniature organ that mimics the functions of a real organ. It has since successfully created human lymph organoids that can generate human antibodies.
Organovo, another 3D printing pioneer, went one step further in scaffold-free bioprinting technology and is now one of the most established companies in the field. Its idea, different from all other related companies, relies on the native programing of cells.
Organovo uses multicellular aggregates as bio-ink. When cells are architecturally positioned and stabilized by bio-inert hydrogels, the presence of specific cell types and the cell-cell contact can generate a local environment that mimics in vivo conditions to achieve enhanced tissue-specific functions.
The liver organoids it produces reach a few millimeters thick and can survive in vitro for about one month.
These 3D-printed organoids are used as animal model substitutes for drug tests, which could significantly reduce the failure rate for clinical trials. The goal of the company is to make liver tissue patches the size of an iPhone for transplant in the next 10 years.
Because 3D bioprinting is the most active direction in the custom organ industry, other companies are making shifts from their original courses.
United Therapeutics, a biotech that mainly developed medicines for pulmonary arterial hypertension, announced its collaboration with 3D Systems in early 2017 to launch a multiyear project on printing solid organ scaffolds. The company also released a longer-term pipeline for developing several transplantable organs, including heart and lung.
Putting Hearts on a Chip
Aside from building a full-size heart, the cardiac microphysiological system (MPS), or “heart-on-a-chip,” is another direction in the field. This consists of a cell chamber with three-dimensional cardiac tissue that has microcirculation channels to mimic the nutrient/oxygen transport in a real heart. Like the organoids, heart-on-a-chip is a safer and more effective way to assess the effect of different drugs.
Kevin Healy’s group at UC Berkeley developed a heart-on-a-chip using human iPSC-derived cardiac muscle tissue. After loading the cardiomyocytes to the chip at high packing density and low pressure, the cells form 3D cardiac tissue within 24 hours and start to beat in a uniaxial manner after about a week. Pharmacological data derived from these MPS are more physiologically relevant than those from 2D cell-based studies.
Jennifer Lewis and Kevin K. Parker from Wyss Institute, Harvard University also reported the first 3D printed heart-on-a-chip with soft strain sensors. The soft strain sensors have micro-grooves on the surface that can guide cardiac cells to self-assemble into physio-mimetic cardiac tissues.
The contraction of those cardiac tissues will cause bending of the soft sensor, thus inducing a change in the resistance which could be translated into detectable signals.
Tara Biosystems, a heart-on-a-chip startup in New York City, recently closed on its $9 million series A financing co-led by Trancos Ventures and Morgan Noble, to launch its first products in 2018 and accelerate the development of cardiac tissues and disease models.
Looking Ahead
Despite the increasing interests in custom organ research and the immense investment in R&D, it may still take decades before transplantable lab-grown organs are generated.
The U.S. Food and Drug Administration (FDA) regulations for approvals will also certainly play an important role in determining when the first transplantable organ can be used in patients.
Looking forward, there are many potential directions, such as lowering the cost and risks of clinical trials and developing personalized drug screens and therapies. As the frontiers of science inexorably expand, obstacles to these technologies are giving way, and this holy grail of medicine, custom organs, is slowly becoming attainable.
