Zika: How to fight back
There is no putting the Zika genie back in its bottle, but there are quite a few things that can be done to thwart its progress.
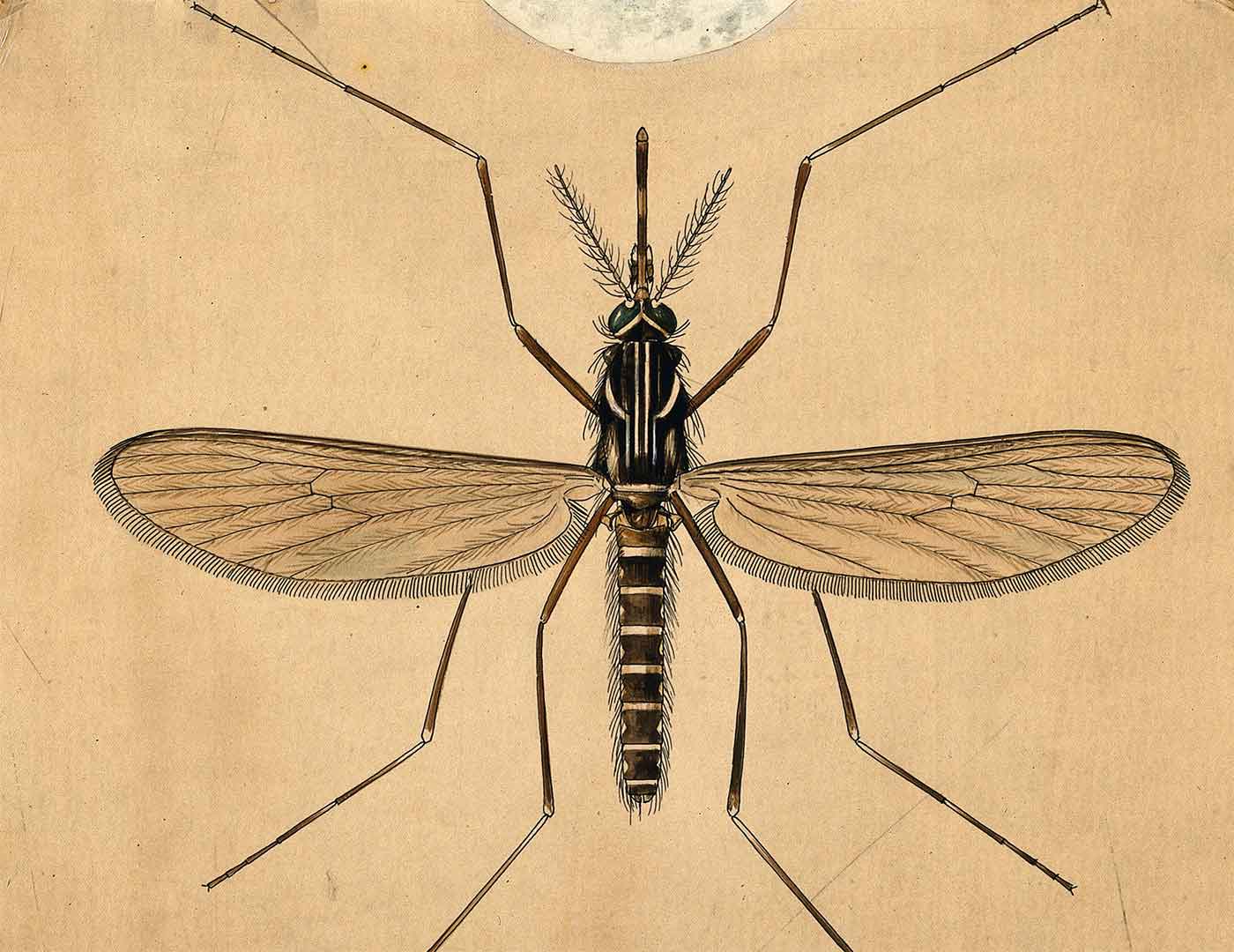 A mosquito (Aedes aegypti), by A.J.E. Terzi. (source: Wellcome on Wikimedia Commons)
A mosquito (Aedes aegypti), by A.J.E. Terzi. (source: Wellcome on Wikimedia Commons)
Background
Zika, a virus associated with shrunken heads in babies and creeping paralysis in adults, seems more science fiction than science fact, but it is all too real and all too heartbreaking. Its insidious ability literally to attack the future by targeting the unborn sets it in a category all its own. Yet, the outlines of the Zika story were familiar to me. Seventeen years ago, another mosquito-borne virus from Africa appeared out of nowhere, leaving a bewildering array of destruction in its path: flu-like illness; encephalitis; paralysis; and the most unexpected, and therefore the most unsettling of all, a trail of dead crows.
When West Nile Virus (WNV) first appeared in New York City in the summer of 1999, the Centers for Disease Control (CDC) blew the diagnosis, chalking it up to a related virus, St. Louis Encephalitis. It took a veterinary pathologist with a freezer full of dead birds at the Bronx Zoo to connect the dots and prod the CDC to keep looking.
The following spring, I trailed a team of wildlife biologists tracking birds migrating up the Mississippi flyway for a story on how the virus was quickly spreading across North America. For West Nile, birds are an “amplifying” host, brewing up enough virus to infect mosquitoes, driving the cycle of disease. That dozens of other species, including humans, could also become sick was unusual. That dozens of mosquitoes species could vector (transmit) the virus was gobsmacking.
For Zika, primates are in the bird role, capable of generating enough virus to infect mosquitoes that, in turn, infect more primates. A single infected mosquito can spread the disease to several people through serial bites in her quest to amass enough blood to nourish eggs, which are typically laid in batches, called rafts, of a 100. So far, the primary mosquito suspect is Aedes aegypti, also of African origin and with a special taste for humans. Its cousin, albopictus, also known as the Asian Tiger mosquito, is yet another invasive and also thought to vector Zika. In the lab, Culex mosquitoes, which are far more common, may be involved as well. With billions of mosquitoes and hundreds of millions of susceptible people to keep them fed—and nary a screen to separate the two—Brazil provided a perfect storm of virus, vector, and victim.
Adding yet another strange twist to the story, Zika can also be transmitted by sex, a fact made even more treacherous because in most cases—as many as 80%—there are no tell-tale symptoms of infection. Lacking good diagnostic tests, it can be impossible tell who is infected. Ratcheting up the danger another notch, Zika can lurk in semen for a staggering two months.
However, just because a virus can spread does not mean that it has to. Like all infectious diseases, Zika is a numbers game:
- If there are enough mosquitoes infected with the virus and capable of transmitting it (not all mosquito species can)…
- If enough of these mosquitoes actually bite people (not all do)…
- If enough people then develop enough virus to infect mosquitoes back…
- Then the cycle will continue and the epidemic will spread.
Anything that disrupts any part of the cycle breaks the chain, lowering the incidence of disease.
Arrows in the quiver
There is no putting the Zika genie back in its bottle and no silver bullet solution, but there are many things that can be done to slow and even control its spread. Some solutions focus on the means of transmission, some on methods, and others on opportunity. The winning answer is a medley that balances effectiveness, low cost, and ease of deployment, along with minimal collateral environmental damage.
Barriers
Screens: Sometimes the best answer is a simple one: short circuit the problem. In 1854, public health and epidemiology pioneer John Snow removed a water pump connected to a contaminated source and stopped a cholera outbreak cold. Similarly, window screens would go a long way toward keeping mosquitoes and people apart. Remarkably, screens are not a given in Brazil, a fact that startled many when the organizing committee for the Rio Olympics offered to install them in team dorms for an extra fee.
In an article for The Daily Beast, journalist Martha Mercer writes of her travels to Brazil:
In the bathroom, they (mosquitoes) favor the mirrors and humid shower stalls. In the bedroom, they lie in wait under the bed and inside the wardrobe. A thump on the sofa will always launch a few into the air in the living room…
…The Brazilian government recommends screens as the most effective method to protect against the insects, but aside from the occasional bedroom window, screens are nearly nonexistent here—no matter how wealthy the inhabitant.
When I arrived in December with my husband and toddler son to spend a few months with family, one of our first items of business was to find someone to build frames for the rolls of screen we had brought with us. We thought it would be simple. Six weeks later, we still haven’t found anyone who knows anything about screens.
A system of inexpensive, easy-to-install, easy-to-repair screens, adaptable to any window size, would make a big difference—not just for Zika, but also for dengue, chikungunya, yellow fever, and other mosquito-borne diseases.
Repellents: For years, the “go-to” answer for repellents has been DEET (N,N-diethyl-m-toluamide), a compound developed by the U.S. Army to protect soldiers from a variety of mosquito-borne tropical diseases while fighting in the jungles of the Pacific during WWII. It took more than a half century before researchers began to tease out exactly how it worked. The mechanics are different, but basically it is the Febreze approach, turning mosquitoes “nose blind” to the scent of humans. Over time, some insects have evolved around it, while others, including Aedes aegypti mosquitoes, have proved naturally less susceptible.
Picaridin (aka, Icaridin) at 20% solution also ranks high on the World Health Organization’s (WHO) list of repellents, but its effectiveness can vary among different mosquito species.
That leaves a raft of natural repellents—such as oils derived from citronella, eucalyptus, lemongrass and geranium—and, according to researchers at New Mexico State University, a perfume called, of all things, Bombshell. Effectiveness varies and can be reduced simply by sweating.
Inspired by the insight of DEET mechanics and armed with Grand Challenges funding from the Bill and Melinda Gates Foundation, Vanderbilt University’s Laurence Zweibel has been experimenting with a new kind of repellent designed to overload an insect’s sensory circuits. Rather than selectively turning sensors off, his scheme turns them all on. Zweibel’s team has come up with a compound called VUAA4 (Vanderbilt Allosteric Agonist 4), which they plan to embed into a plastic wristband wearable powered either by a battery, a solar cell, or even a person’s movement. VUAA4 would be released into the air, creating a personal no fly (or mosquito, tick, flea, or louse) zone: a chemical bubble of protection.
VUAA4 offers the possibility of an extraordinary all-in-one solution to keep a variety of biting, sipping, and generally annoying insect pests at bay. For the very same reasons, the potential for collateral damage is significant if used in large-scale applications such as agriculture or lawn care. Although the compound does not kill insects, a treated field or yard could present a daunting barrier to migrating insects such as butterflies, or force bees to waste precious energy flying around it in the quest for nectar. A treated field or garden would also keep out beneficial insects such as ladybugs, raising the alarm of potential ramifications up and down the food chain: Silent Spring redux.
Still, a personal anti-insect cloaking device has its charms.
Vaccines: The ultimate protection against a disease is an effective vaccine, and at least a dozen teams from all over the world have jumped into the race to develop one for Zika, according to the WHO. Unlike Ebola, the virus was not a priority before the outbreak, so nothing was in the research pipeline, but work on dengue, a related virus, has provided a solid first step for French pharmaceutical company Sanofi | Pasteur and the U.S. National Institutes of Health.
There are several ways to build a vaccine. Traditionally, the two most popular have been to use a live attenuated (weakened) virus or an inactivated (dead) virus to trigger an immune response priming the system for an actual assault. Another way around this is to pack viral genes with strings of DNA called plasmids to generate virus-like particles that are neither alive, nor dead.
Once an effective vaccine is developed, the next problem is delivery. They must be able to remain stable in warm tropical temperatures. Vaxart, a San Francisco-based biotech, is working on a vaccine tablet that would make deployment easier and possibly cheaper: no cold chain, or syringes, required.
To help speed up the development process, Zika has been added to the list of diseases eligible for fast-track FDA vaccine review. Even so, although trials for some of the candidates are slated to begin as soon as this fall, it will take several years to complete clinical trials.
Pregnant women, arguably the cohort most in need of a vaccine, are generally ineligible for trials since the maternal immune response itself may present a threat to an unborn child. Fetal exposure to a handful of viruses has been linked to an increased risk of children developing a mental illness later in life. A maternal response to the flu virus, for example, has been associated with an increased risk for schizophrenia. The virus itself does not cross the placenta to infect the fetus, but small proteins that are integral to the immune response called cytokines can. Add to the list of known unknowns: an understanding of the mechanics of prenatal Zika infection.
Another hurdle is a deep, embedded distrust of the Brazilian government. Rather than Zika, some are convinced that a bad batch of vaccines given to pregnant women are responsible for the increase in microcephaly cases. In fact, Brazil has many potentially overlapping health crises, and the lack of consistent medical record-keeping not only has made it more difficult to tease them apart, but has provided fertile ground for rumors to root.
Intel
Diagnostics: No one yet has clear handle on the most basic metric of the outbreak: how many people have been infected with Zika? Without an accurate, simple, and inexpensive diagnostic kit, there is simply no way to know.
Likewise, there is no way to know how many people have developed natural immunity after exposure to the virus. A “herd” immunity develops when enough people develop natural immunity, breaking the cycle of infection back to mosquitoes.
There are other benefits. Women who had a way to know if they have natural immunity could cross Zika off the list of things to worry about during pregnancy. Conversely, if men had a way to know whether they were infected, they could take steps to keep their sex partner(s) safe. Add condoms to the list of low-tech barriers.
The FDA has also fast-tracked review of diagnostics—with the first, a triple test for Zika, dengue, and chikungunya, just approved for distribution to a special network of labs that respond to public health emergencies.
Big data: Good diagnostics are also essential for compiling data to help uncover risk factors, especially for conditions that are comparatively rare. For example, sophisticated data analysis could help tease out clues explaining why some people develop Guillain-Barré Syndrome, a creeping paralysis that affects adult patients. Do serial and co-infections with other viruses such as dengue play a role?
Screening: At present, there is no way to test for Zika infection in blood donors. Even if a donor is either pre-clinical (it takes about a week after infection for symptoms to appear) or asymptomatic, enough virus could be circulating in their blood to pose a threat. So serious is the issue that the U.S. Department of Health and Human Services has begun shipping blood products to Puerto Rico, where 100,000 cases of Zika are predicted, to guarantee a safe supply.
Research teams all over the world are working not only to develop ways to screen for Zika in blood, but also in urine and saliva. Until those tests are ready, efforts to map Zika’s spread, including Google’s recently announced $1 million collaboration with UNICEF, will be severely limited.
Vector control
Killing the messenger is an obvious choice: no mosquito, no bite, no problem. For the last 225 million years, possibly longer, the only species that have liked mosquitoes are either those they pollinate or those that eat them. For everybody else, the whine of a female on the prowl for a blood meal—a sound older than the Himalayas—has inspired everything from annoyance to despair. Mosquitoes have survived at least two great extinction events, including an asteroid impact that briefly boiled the Earth’s atmosphere. They have blossomed into more than 3,500 species, although only a fraction (about 200) bite humans. It seems unlikely that they can be eradicated.
That doesn’t mean they can’t be fought.
Chemical warfare: Along with the image of a very pregnant woman, an infant with a painfully tiny head, and a close-up of a blood-engorged mosquito, the image of a man in a moon-suit and Darth Vader respirator with a fogger system strapped to his back has become an icon of the crisis. At best, however, pesticides, most of which contain a version of a synthetic chemical called permethrin, kill about half the mosquitoes targeted. The rest either survive tucked into tiny places safe from fogging, or buzz blithely on, resistant to the poisons swirling around them.
Larvicides—chemicals added to standing water to kill larvae—work. But when a single Aedes aegypti mosquito can lay a raft of eggs in a capful of water and every puddle has the potential to serve as a nursery, there is a limit to what can be done.
Traps: Build a better mosquito trap and the world will beat a path to your door. The basic idea is simple: a container with water that looks like an ideal mosquito nursery, but is instead an insecticide-laced prison from which there is no escape. Production of Seattle-based Springstar, Inc.’s aptly named “Trap-N-Kill,” a $9 trap based on technology originally developed for the military, is quickly ramping up, driven both by the Zika scare and an outbreak of dengue in Hawaii. However, to really make a dent in the problem, larger traps are needed that can be replaced every couple of months, instead of every couple of weeks.
Research in Puerto Rico on “hay traps” has been promising. A packet of hay is dropped into water in a five-gallon bucket. The heady aroma of decomposition lures females to fly through an opening in the lid where they are then caught on sticky paper and die before any eggs can be laid.
Long-term field tests have shown a reduction of local mosquito populations by nearly 80% compared to neighboring areas. Success requires the participation of the majority of residents: three traps per house with permission for government workers to come onto private property to maintain the traps.
Although the traps are effective, mosquito populations still bump up after rains, just not as much. Notably, the traps trapped both Aedes aegypti and Culex quinquefasciatus mosquitoes. the latter have been shown in the lab to be capable vectors of Zika.
Gene warfare: The goal here is to crash a population, and there are three main ways to go about it.
The first is radiation, championed by the International Atomic Energy Association (IAEA). Sterile Insect Technology (SIT), as it is known, has a long and successful history battling a variety of agricultural pests. Male mosquitoes—plant pollinators who don’t bite—are exposed to X and/or Gamma rays to make them sterile, then released into the wild to mate. The eggs, of course, don’t hatch and the population plummets. For the scheme to work, however, irradiated males must outnumber the local boys by a factor of 10 or even 20 to 1. Field tests have shown dramatic reductions in mosquito populations of 80% and more, but it takes millions of lab-raised mosquitoes to make a dent.
British biotech Oxitec (recently acquired by U.S.-based Intrexon for $160 million) takes a more targeted approach to SIT, inserting a self-limiting gene into lab-bred male mosquitoes. When released to mate with wild females, the offspring survive, but die before they are old enough to mate. Field tests have also shown dramatic reduction in mosquito populations. Recently, the FDA ruled that that genetically modified (GM) mosquitoes do not present an environmental threat, paving the way for a test in Key West.
Since a single female mosquito can lay hundreds of eggs in her short lifetime, populations rebound, making repeated releases of sterile males necessary. According to an estimate in Technology Review, the Oxitec system could cost $7.50 per person per year, a tally that would quickly spike into hundreds of thousands or even millions of dollars per year, per city. Irradiation is likely to be less expensive and, with IAEA at the helm, the technology is more readily shared.
Another option is to insert a “kill gene” using a highly specific technique for genomic editing called CRISPR/Cas9. In a nutshell, it shortcuts natural selection by making sure that all copies of a specific gene passed down to offspring are identical, rather than the traditional range offered by the mix of maternal and paternal versions. Inserting a gene, for example, that would ensure that all offspring would be male would quickly skew population demographics as it spread throughout a population, spelling doom within a few generations. The scheme has already had success in the lab.
Beyond the ethics of an engineered extinction, nature abhors a vacuum. New populations of mosquitoes would eventually move into a vacated niche and the whole process would have to be repeated.
Germ warfare: By comparison, infecting populations of mosquitoes with bacteria or viruses seems almost old fashioned, but may prove the most effective and lowest cost option.
Several teams all over the world have been working for years on projects to adapt Wolbachia, a natural insect disease, to Aedes aegypti mosquitoes. The bacteria would make it more difficult for them to transmit pathogens. In other words, it would make them just sick enough to not make us sick.
It also affects fertility, so there are fewer mosquitoes. When infected males mate with healthy females, eggs don’t hatch. When infected females mate, offspring are born infected. The hope is that Wolbachia can establish as a self-sustaining system. If a new population of the same species of mosquito were to move into the area, they, too, would soon be caught in the Wolbachia trap.
Researchers are testing out various methods of deployment. In a field trial currently underway in Townsville in Queensland, Australia, to control Aedes aegypti mosquitoes carrying dengue, thousands of volunteers are raising and releasing batches of 100 infected male mosquitoes in their backyards. If this works, the cost to protect the city of 170,000 people would be roughly 50 cents per person.
The Eliminate Dengue project team from Monash University—another effort funded by the Gates Foundation’s Grand Challenges program—is also working on projects in Brazil and Colombia.
Taking a somewhat opposite tack is Xi Zhiyong, a professor at both Sun Yat-sen University in China and Michigan State here in the U.S. He has built a 3,500 square-foot mosquito breeding facility, the world’s largest, in Guangzhou, capable of producing 20 million Wolbachia-infected male mosquitoes per week. Within 10 years, production is expected to ramp up to 2.5 billion weekly, with the goal of eliminating Aedes mosquitoes in cities across South China. Last year, a test involving serial releases on Shazai Island proved so successful, only a single larva hatched from the eggs collected in the sample area.
Zhiyong’s work is largely funded by the Chinese government, but notably it, too, received Gates’ funding when the project started up five years ago.
Viruses may provide yet another line of attack. Scientists have identified naturally occurring densoviruses that target different species of mosquitoes, including Aedes aegypti. These show promise as larvicides, but even mosquitoes that hatch live lives too short to cause any trouble. Research is not nearly as far along as for Wolbachia, but along with another possible solution comes the bonus of poetic justice: a virus to vanquish a virus.
And the kitchen sink
No organization has come close to funding as broad a range of ideas for whacking mosquitoes than the Bill and Melinda Gates Foundation. In 2007, the foundation launched the Grand Challenges Explorations program specifically to support “high-risk, high-reward proposals” to address a broad range of urgent public health issues. The mosquito research has primarily been focused on ways to control malaria, but often can be applied to other mosquito-borne diseases.
Some of the schemes seem more appropriate for a grilling on ““Shark Tank”“, such as the eMosquitoNet, “which plays music that includes sound waves at resonant frequencies of female Aedes aegypti mosquitoes…causing uncontrollable vibrations and a failure of the mosquito’s navigation system.” While that may turn out to be Death by Britney Spears Greatest Hits, it sparks a new line of thinking: can sound waves be used as a deterrent?
Another project, led by Columbia University physicist Szabolcs Márka—whose day job involves tracking gravitational waves—uses a solar-powered rod emitting ultrasound waves to kill mosquito larvae. He has also prototyped a “light curtain,” tuned to frequencies that befuddle bugs so they stay away.
It it well worth scrolling through the list of Grand Challenges projects for inspiration. Unfortunately, no follow up reports are provided, so it is difficult to know which projects have seen success.
Mosquito planet
In many deeply profound ways, our battles with mosquitoes and the pathogens they carry have marked our history. Outbreaks of malaria contributed to the fall of the Roman Empire. Mosquito-borne “fevers” slowed the advance of European settlers into the New World and provided strategic advantage in Haiti’s fight for independence. An all-out war on mosquitoes made the Panama Canal—and modern global trade—possible. DEET helped the Allies win WWII. It also made it feasible to send more than eight million American troops to Vietnam.
Less than a century ago, in 1922, tens of thousands of cases of dengue were reported in the states surrounding the Gulf Coast. Screens, air conditioning, massive water projects, and the use of DDT (fraught though it was) made the post-war boom years possible. Today, Texas and Florida rank second and third for population with a combined total approaching 48 million. Tens of millions more flock to the regions as tourists each year. If mosquitoes and the diseases they carry were to stage a comeback, that all comes to halt. The stakes are as high as they can be.
The point is that nowhere can be safe until everywhere is safer. Tropical diseases are not just for the tropics any more. When a “footnote” pathogen such as Zika, discovered almost by chance nearly 70 years ago in a forest in Uganda, can emerge halfway around the world in Brazil, spread quickly and cause such widespread devastation, then we have to take a good long look at what we are doing that helps make that possible. More footnotes are out there, poised for the next time the stars of vector, victim, and virus align.
