The Information Technology Fix for Health
A tour of technologies, tools, and trends to help you understand the state of information technology and health care.
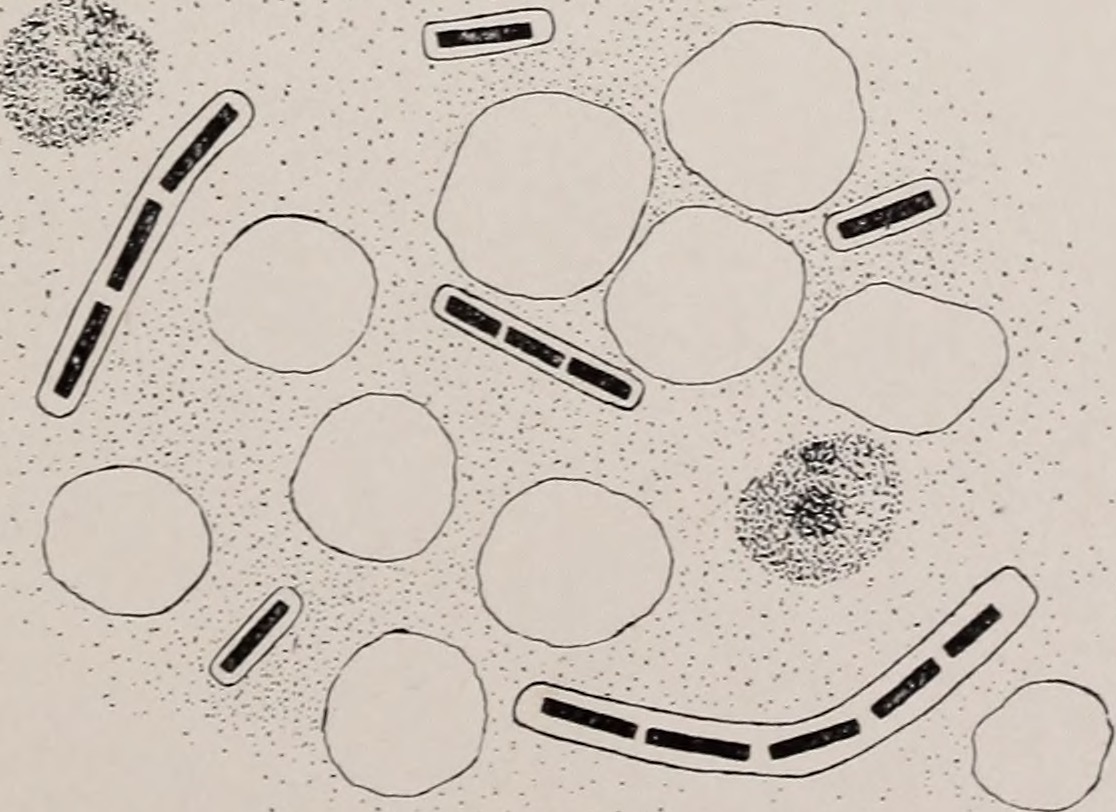 Addresses and papers (source: Internet Archive Book Images)
Addresses and papers (source: Internet Archive Book Images)
Barriers and Pathways to the Use of Information Technology for Better Health Care
A constellation of new health-related activities and technologies, validated by clinical research and starting to roll out into medical practice, holds the promise of better health for everyone. These activities exploit the astonishing miniaturization of ever-more powerful devices, along with the collection, analysis, and sharing of data, to support better coordination and delivery of health care. Interest in these innovations is driven by the health care system’s pressing need to:
- Control chronic illnesses such as diabetes and hypertension to prevent progression and complications
- Find more effective and less intrusive treatments for a range of diseases, and do so faster
- Lower system-wide costs, or at least staunch the rate of increase
- Reduce medical errors and misdiagnoses
- Improve patients’ sense of control over their care and their destiny
- Ease stress on practitioners and caregivers
- Sweep away some of the administrative and bureaucratic load
What are the promises of the new technologies, and what conditions have to be in place to enjoy those benefits? Why do some technologies seem to languish despite their apparent advantages? How do all these things depend on each other, and what technologies and activities need to be adopted in tandem?
The large trends in these groundbreaking approaches—as well as the things that stand in their way—form the subjects of this article. It is not a catalog of applications or technologies, but a broad investigation of their potential. I hope that the themes herein come home to several types of diverse readers:
- Anyone with a career in medicine and the enormous health care industries will see big changes in the field. The health care industries aren’t likely to shrink dramatically or be disintermediated as have travel agents, bookstores, many newspapers, or much of the music recording industry, but some of their functions will disappear while others leap into the twenty-first century. The technologies discussed here will be implicated in these disruptions.
- Computer experts, data scientists, and other hi-tech professionals will stream into health care, where they will stumble upon very unusual activities and norms.
- Professionals in public health and health care policy will want to understand the potential the technology holds to affect treatments and costs, and to maintain a clear-sighted view of the problems that crop up when applying the technologies. Problems are unknown to or underestimated by some observers, while being shaken vigorously in our faces by others to block the deployment of useful technologies.
- People concerned about the economic future of nearly any country in the world should worry about the exploding costs of health care. These are being driven by aging populations as well as new diagnostic techniques and treatments that provide astonishing advances in extending human life, but at great expense, and are exacerbated by inefficient business and clinical processes, lack of information liquidity, and overlapping, sometimes contradictory regulatory demands. Smart health technologies, including patient engagement, could help those increases to level off.
- Everybody will feel the shift. Your interactions with this new health care system (and for the first time, we might really be able to ennoble our grab-bag of medical practices and technologies by calling them a “system”) will differ depending on whether you are young or old, live in a city or the country, are (currently) healthy or chronically ill—but the interaction will be very different from what most people have now.
What are some of the technological changes coming over the horizon?
- Sensors are checking how elderly residents move around their homes, and registering signs of inactivity that may indicate ill health or atypical patterns suggesting disorientation.
- Behavioral conditions are being treated with the help of games, some of which produce lasting improvements such as promoting adaptation in victims of PTSD, and instilling control in people with ADHD by presenting tasks and then throwing distractions at the player.
- Large-scale data analysis of patient reactions to marketed drugs are turning up adverse effects not found during clinical trials, and prompting reconsideration of the sterling trust placed in conventional trials.
- Electronic record exchange is allowing patients to walk into a hospital hundreds of miles from where they have previously been treated and offer unfamiliar doctors complete medical histories, including key information such as drug allergies.
- Mobile phones are allowing people in isolated rural areas, even in developing nations, to snap photos of medical problems or even measure vital signs and get advice from remote doctors.
- Researchers are starting to release not only articles about their research, but also the underlying data used to reach their conclusions, allowing other researchers to check their work, duplicate studies, and combine the data from multiple experiments.
Technology is always just a tool, whose use rises, falls, and metamorphizes through its relation to the people and organizations that use it. Technology also introduces risks whose effects in medicine can weaken the doctor/patient relationship and cause life-threatening errors. Although this article does not delve into social policy or organizational change, I’ll look at some of the impacts these have on the technologies, and vice versa.
Health reformer Arien Malec delineated (in a video-taped presentation) the tension between technology and the personal touch. In earlier ages of medicine we enjoyed a personal relationship with a doctor who knew everything about us and our families—but who couldn’t actually do much for us for lack of effective treatments. Beginning with the breakthroughs in manufacturing antibiotics and the mass vaccination programs of the mid-twentieth century, medicine has become increasingly effective but increasingly impersonal. Now we have medicines and machinery that would awe earlier generations, but we rarely develop the relationships that can help us overcome chronic conditions.
Health IT can restore the balance, allowing us to make better use of treatments while creating beneficial relationships. Ideally, health IT would bring the collective intelligence of the entire medical industry into the patient/clinician relationship and inform their decisions—but would do so in such a natural way that both patient and clinician would feel like it wasn’t there.
This article takes a tour through specific technologies, tools, and trends to see what has really been accomplished and what is feasible in the near future:
- Devices, sensors, and patient monitoring
- We start our journey with information technology that lies right next to our bodies, and sometimes even inside them. This section discusses how things we touch, hold, and wear, along with our concern for fitness in daily life, can become part of formal health treatment.
- Using data: records, public data sets, and research
- The use of computers, including the devices from the previous section, revolves around data. Here we turn to an area of information technology that is somewhat hidden away but will prove absolutely crucial to health care: understanding ourselves through data about ourselves and our institutions. This must be collected, stored, sent between health care sites, and used to find better treatments.
- Coordinated care: teams and telehealth
- Fortified by the background in the previous two sections, we can proceed to changes taking place in treatment settings, including new ways of structuring teams and even sets of health care institutions, and where these institutions need to draw on the technologies discussed in the article.
- Patient empowerment
- People stand front and center throughout this survey of technology. The article will culminate in the empowerment that information technology offers people on their own or when engaging with the health care establishment.
Devices, Sensors, and Patient Monitoring
When many people think of medical devices, enormous clanking machines that might cost a million dollars or more come to mind (such as for radiology, MRIs, CT scans, or lab analysis). The output from these devices tends to pass through labs, radiologists, or other medical oracles while the patient chews her fingernails and waits several days for results. But as in other technologies, miniaturization is transforming medical equipment. Lots of small devices are already in use, with pacemakers and other cardio implants bringing dramatic improvements to quality of life. Other devices bring health data into the hands of ordinary people—even turning up in smartphones.
Digital Building Blocks of a Health Plan
Attendees at the high-profile Consumer Electronics Show at the beginning of 2014 lost themselves in a sea of personal monitoring devices. Whether or not these early consumer devices take off, self-monitoring is on the verge of becoming mainstream, with the use of apps expected to expand rapidly. Gadgets marketed to consumers can bypass many of the barriers to development, regulatory approval, and marketing that currently keep devices expensive and focused on a single task.
Technologies supporting the Quantified Self movement include the following:
- Fitbits and other wearable measurement devices are surging in popularity. Just walk through a consumer electronics store to see how widespread and available these devices are. Many measure not only activity, but also health-related vital signs such as pulse, blood pressure, and oxygen consumption.
- Devices are becoming easier and friendlier to use. For instance, the HeartCheck Pen is a small, pen-sized device that takes readings from the thumbs when pressed onto the sensor pads—a device of potential value to people at risk for stroke and heart attacks. The Nymi is a bracelet that measures one’s ECG from the wrist and fingertip. Diabetes patients need to measure glucose levels frequently and manage insulin dosing to prevent hyperglycemic complications and avoid hypoglycemic episodes, so noninvasive measurement devices now avoid the need for frequent skin pricks—one such device is embedded in a contact lens. Although currently positioned only as an authentication technology (a security device to replace passwords), the possible medical applications of a mobile device that measures ECG for things such as cardiac disease monitoring are exciting.
- Wristbands and finger clips may soon seem quaintly awkward, with even greater miniaturization on the way. Reductions in size democratize medicine in many ways: by lowering the costs of devices, by making them more attractive and comfortable (a critical consideration for widespread adoption), and by reducing power requirements. For example, sensors warning of concussions can be worn under sports helmets or embedded directly in them, although their accuracy is disputed.
- Sensors embedded in pill containers can notify doctors when the patients have taken their medication. This can help clinicians remind patients and encourage medication adherence, which is a major problem in maintaining health because so many patients forget their pills or need urging to adhere to their regimens. If smart packaging sounds like science fiction, just consider ingestible pills that work together with a body patch and a smartphone to signal when they’re digested.
- A chip small enough to be sent through blood vessels returns ultrasound measurements of the vessels or the heart. Researchers expect to shrink it further.
- Robots can be seen increasingly roaming the hospital corridors, and will eventually turn up in nursing care facilities and even the home as well.
People use personal devices to measure improvements in personal goals and bolster their determination to achieve even more (although as we will see, most of the devices and apps are not used for very long). Devices also connect people with others engaged in fitness programs and form communities for support.
Although some people can benefit individually from reading and interpreting the displays on their devices, the data is most valuable when inserted into a patient record and combined with data from other users. In a patient record, the data can be checked by clinical experts and be mined for trends. Combining data from many users enables such benefits such as finding out where they stand relative to the population as a whole. Are you better or worse off than the norm? Are your vital signs in a danger zone?
Environmental Sensors: Where Do You Feel the Pain?
With mobile phones and dedicated consumer devices to support the quest for health, the trend today is to manage chronic conditions, the difficulties of aging, and recovery from traumatic events and surgery—really, anything that benefits from close attention by clinicians—in the environments where the patients spend their time. And what could make more sense? After all, the patient’s symptoms occur in the environment where he spends his time. The Institute for the Future writes, “Health care is moving from an acute, episodic care model to a more continuous, chronic care model” (page 7 of the paper). That paper also lays out the move from the professional setting to the patient’s environment, and the crucial role that will be played by mobile devices and sensors in the hands of patients.
Dueling trends are at work as devices bring the clinic into the home. On the one hand, consumer devices are unfolding the vision expressed by health IT leader Samir Damani: “We are really moving from a doctor-centric society to a patient-centric society.” On the other hand, sensors can be scary and intrusive. Obviously, consumers will rebel against monitoring unless their privacy is respected and they feel like partners are improving their own health with the support of the clinician and technology.
The home is not the only place that can join the clinic and the hospital as health settings—other important places in people’s lives, such as schools and workplaces, can as well. Public interest in health tools outside clinical settings is growing worldwide.
Barriers to Devices and Sensors
In addition to personal or cultural aversion, the barriers that hold back adoption of sensor technologies include the following:
- Efficacy
- It takes a long time and a lot of money to develop a medical treatment, and sometimes even more time and money to establish that it’s safe and works better than a placebo. Small devices present fewer headaches than drugs because any safety problems they pose are likely to be concrete and obvious. Clinical trials for devices are much simpler than drug trials for a host of reasons, ranging from the high failure rate of new chemical compounds to the more straightforward safety considerations of external devices.
Still, to line up people with the right combination of medical conditions, ensure they follow instructions, and measure effects (especially over a long time period) is a big job. Given so many competing, poorly-tested apps, most fail to appeal to users or to be particularly effective. Few are downloaded by a lot of people (for instance, only 1.2% of the smartphone-enabled diabetes population uses apps), and far fewer are used over a long period of time. This resistance holds back market penetration, makes it hard to gather statistically significant measures of their efficacy, and dampens investors’ incentive to improve products.
Although most manufacturers of the current generation of consumer devices are careful to label them for “fitness” rather than “health,” there is a point where their use can trespass onto the realm regulated by government. The FDA has even declared jurisdiction over mobile phone apps that have clear medical purposes and has reviewed more than 100 such apps, although the agency is doing its best to keep its hands off popular devices and apps for casual use. Its regulatory jurisdiction extends over devices used for diagnosis or treatment of specific medical conditions, not health in general.
- Cost
- If we can save lives and avoid emergency room visits or other costly treatments, a medical device comes cheap at almost any price. FDA-approved cardiac devices and other implants have established themselves as cost-effective. But no one can guarantee that the emerging generation of consumer and patient devices really does what people fervently hope them to do. In the meantime, most people (and their insurers) still think twice before buying a gadget of unclear value.
- Data quality
- Different devices can report different measurements, raising suspicions about their trustworthiness. Each device may produce information that’s useful in a relative sense (i.e., how much the value goes up and down over time) but perhaps not useful in its absolute values.
- Simplicity
- Consumers who are content to spend days setting up a home entertainment center seem to lose patience when it comes to devices that improve their health. If the interface is more than a single button, many will give up at the start. Simplicity must also be the rule in displays. It’s particularly important for the elderly (who did not grow up with ubiquitous computer technology) and for anyone injured or impaired (chemotherapy and dementia are just two of the burdens that affect one’s ability to remember and follow technical instructions).
- Overmeasurement
- People can get compulsive when measuring themselves, and overinterpret arbitrary changes that take place day to day or hour to hour. Measuring your blood pressure can raise your blood pressure! Throwing data into a bucket doesn’t improve our knowledge; we should determine our goals first and then collect the data that we can process to help reach the goals.
- Interoperability
- When a home or the hospital room contains multiple sensors and devices, they need to work together to contribute to a holistic view of a patient. Some standards exist to help devices communicate, such as the Data Distribution Service (DDS), MQ Telemetry Transport (MQTT), and Extensible Messaging and Presence Protocol (XMPP). In an age where coordinated systems keep airplanes on course, it’s ridiculous that most medical devices are not designed to work with other devices.
- Integration with records
- Before data can enter patient records, systems must be designed to gather well-structured patient data, and appropriate privacy and security controls must be in place. Few electronic health systems currently accept data directly from patients, who still fill out paper forms to be entered by clerks into electronic formats. Furthermore, patients will be tempted to falsify data under some circumstances (such as to earn the incentives dangled by employee reward programs), so there must be technical measures to prevent tampering with device output. Some clinicians mistrust patient-generated data, even though most of the information in clinical interviews comes from patients anyway.
An Endeavour Partners white paper found that one-third of people who buy wearable devices give them up within six months, and half within two years (page 4). This is not necessarily bad: perhaps the users felt that their use of the devices during that short period was sufficient to meet their goals, such as losing weight or establishing a regular exercise routine. But in the quest for long-term use, the white paper proposes nine criteria that could bond users to their fitness devices. In addition to psychological factors such as attractiveness, ease of use, and reinforcing the user’s goals, the white paper urges the provision of an API so that data from devices can be integrated.
Self-tracking is certainly taking off. According to a Pew report, 69% of Americans track some aspect of health for themselves or a loved one (although usually without digital devices), and 63% of trackers believe it has had some positive effect. Whether or not tracking was really responsible for the change, believing that it does is a good enough reason to do it. The huge base of Quantified Selfers can give researchers crucial data to isolate the factors that work most often.
Device manufacturers can then base their designs on factors known to be effective, and demonstrate the value of the devices. Finally, the more these devices interoperate and support the integration of their data, the more they can contribute to the larger health system. This system includes the records that will store the data and the research that will mine its insights.
Using Data: Records, Public Data Sets, and Research
Just as we don’t think often about the electrons coursing through most of the tools we use in twenty-first-century life (until the bars on our screen shrink to an alarming low), we don’t often notice the data that connects us. For medical devices, data is paramount because it’s what we want from the devices in the first place. Data injects power throughout the rest of the health care system.
This section will look first at how data is gathered, stored, and analyzed, then at the use of open data sets and the role of shared data in clinical research. All of these initiatives potentially improve health through shared data and its analysis.
Electronic Health Record Systems
Walking into clinics where the staff carry around paper records makes you feel like you caught an old 1930s movie and should be seeing the scene in black and white. Recently, superficial signs of progress have taken hold. Policy makers in the United States boast about the increasing adoption of electronic records, particularly since the roll-out of Meaningful Use incentives in 2009. But don’t jump to conclusions about the capabilities of new electronic systems: many are harder to use than the paper records they replace, and barely more useful for data sharing and analysis.
In the United States, virtually every doctor uses electronic records and exchange for billing, because money is the lifeblood of both the health practices and the payers. But other activities, even something as basic as ordering a prescription from a pharmacy, are done manually.
When clinical patient records do get digitized, they remain what one doctor called an “electronic file cabinet,” separate from all the work of planning and executing care. This article will refer to such documents as an electronic health record (or EHR), because that term is compact and commonly heard. But we must really think of patient records as a critical component of an entire health system that involves a sequence of events with each patient, along with analytics that set the direction of whole collections of clinics and hospitals. And one question running through this article is how health institutions can use the EHR more effectively throughout their operation to support what reformers like to call a learning health care system.
In other day-to-day activities, we’re used to making orders online and preserving data electronically. The same kinds of benefits come from electronic records: easier appointments, expedited drug orders and refills, faster billing and reimbursement, etc.
Looking beyond convenience is the promise of clinical decision support (CDS). Doctors can’t keep in their prefrontal cortexes all the information they need to suggest accurate diagnoses and treatments—even the doctors (grudgingly) admit that, which is why specialists and consultations exist. How can electronic records augment clinicians’ intelligence?
- At the most basic level, record systems emit alerts to warn clinicians of actions they propose that are inconsistent with the data in the records, such as when a patient has an allergy to a medication or the dose seems wrong. Alerts, from cardiac monitors, intravenous delivery devices, and other equipment attached to patients are aimed at nursing staff (and sometimes drive them to distraction, literally).
- Electronic records also prompt diagnostic and reimbursement codes, and suggest drugs appropriate to the data entered about diseases. Unfortunately, electronic systems have not proven able to do this reliably. The Insurance Institute for HIT Safety writes, “CDS appears to pose a slew of medical legal risks…while offering few—if any—protections.”
- The cutting edge of computer support can be seen in experimental software that generates diagnoses when fed patient histories. Such “expert systems” were tried in medicine as far back as the 1980s, but fizzled out in the face of limitations in hardware power, speed, and memory as well as the lack of flexible database technology. With the enormous speed-up in computing and the rebirth of artificial intelligence in the twenty-first century, researchers are trying again to see whether the doctor can be rendered superfluous. IBM’s Watson, which they started to commercialize in January 2014, famously proved that natural language analysis can bring to the surface multiple plausible diagnoses for doctors to choose from. But we should take predictions about the obsolescence of the doctor with a grain of salt.
- A digital health system can help the staff intervene with patients, through such simple measures as reminding them to schedule and come to follow-up visits. These sorts of interventions can reduce the risk of hospitalization among high-risk patients, such as those suffering from diabetes. This is a clear example of technology that supports, instead of interfering with, the relationship between clinician and patient.
- A well-structured record-based system can flag patients at high risk, telling staff where to concentrate their attention.
- A patient web portal can allow clients to make appointments, check results of tests, check for errors in diagnoses or medication lists, and communicate with the staff for nonurgent questions. This is a fairly obvious application of digital technology in an age when most people can schedule car repairs and hotel reservations through websites, but it’s surprising how few clinical practices are capable of such basic online interaction.
- Analysis of large data sets can turn up problems that help agencies improve public health. They can also reduce costs by helping hospitals identify and prioritize high-risk patients (a process called patient stratification). Payers use analytics to define “episodes of care” that supposedly encompass all the treatment a patient needs for a particular problem. This in turn lets the payers define how much to reimburse health providers for treating various patients with the same condition.
Some large institutions—notably the Department of Veterans Affairs, with its famous VistA software, and Kaiser Permanente—have historically created relatively well-integrated health systems that support sophisticated interventions to improve patient health. Their achievements crown long-term processes of integrating multiple hospital systems around the records and training all their clinicians to take advantage of the data tracked by the record systems. Institutions can do this when they shoulder a comprehensive role in patients’ lives, insuring them as well as treating them. They represent the kind of all-encompassing, long-lasting coverage that many developed countries do at a national level, and that we will look at under the topic of accountable care organizations. According to one account, Kaiser Permanente’s four billion dollar expenditure on electronic health records paid off.
Most deployments of electronic health records achieve considerably less, however. Most EHR systems follow an old 1980s model of software development:
- They are entirely proprietary, although standards (which we’ll look at shortly) have been superimposed and are beginning to allow limited innovation in data sharing and analytics. Significant barriers to entry (through regulatory capture and installed bases) have allowed early entrants in the vendor space to lock in large market shares with legacy technologies that are hard for innovators to supplant.
- Most systems predate the Web or use rare technologies such as MUMPS (standardized as the M language), with kludgy and limited workarounds just so that EHRs can meet such basic expectations as patient portals and access by clinicians on mobile devices. More recent entrants in the EHR space, such as Athenahealth and Practice Fusion, have chosen to go all-online (Software as a Service, or SaaS), providing web-based records. They tend to be popular among physicians, but Software as a Service stays in the hands of the software provider and is therefore hard to adapt to individual health providers’ needs.
- Not being standards-based, existing software is expensive to develop, install, and maintain. EHRs’ market has therefore been large institutions with millions of dollars to spend on licenses and millions more on implementation. Until recently, proprietary EHR vendors have totally bypassed the small community and rural providers where digital records could tremendously improve care.
- Many existing record systems have been developed to meet the interests of the hospital and clinic administrators who make out purchase orders and deal with third-party payers, not the interests of clinicians who ultimately have to use the system for patient care. The chief purpose of such EHRs is financial rather than clinical. For instance, some of the “clinical decision support” built in to these systems actually tells doctors how to find the codes that legally maximize the payment for a given course of treatment (a trick called “up-coding”).
- Although digitization has transformed other industries, such as ecommerce and finance, by facilitating data exchange, the long proprietary history of EHRs leaves them stubbornly resistant to interoperability. The standards in this area have improved recently, as we’ll see later in the article. But currently, it is hard even for patients to obtain their own records, on paper or electronically—a right enshrined in law through HIPAA.
The incentives in the HITECH act, part of the 2008 economic recovery act, spurred adoption of electronic health record systems. But improvements in quality through electronic records are more elusive. Although most studies show improvements in care, they turn out to be small and scattered. For instance:
- The Agency for Healthcare Research and Quality (AHRQ) found some decrease in unnecessary tests, and improvements in pediatric care, particularly around prescriptions. But many other areas showed no improvement, or a statistically insignificant one.
- A 2011 article in the Journal of the American Medical Informatics Association also found benefits in medication prescription.
- A New England Journal of Medicine article found that electronic record systems reduced errors in medication, but no evidence that it reduced errors in diagnosis.
Trying to determine the real impact of electronic health record systems is an exercise in frustration. Until recently, most studies were unrepresentative of most EHR use, being based on a few leading institutions or home-grown systems instead of commercially sold systems (see pages 9–11 of this review paper).
It should also be noted that, when trying to measure relative successes and failures, researchers usually define “quality” as how well doctors adhere to recommended standards of care. This is an understandable metric to settle on, because standards of care are precisely defined. It would be much harder to measure how much patients actually improved. But this choice leaves a gap between what “quality” means in clinical research and the “rather simple statement” from the landmark Institute of Medicine book, Crossing the Quality Chasm: A New Health System (page 44): “The ultimate test of the quality of a health care system is whether it helps the people it intends to help.”
The designers of the HITECH act knew that adoption of a technology does not guarantee effective exploitation of the technology’s benefits; that’s why their reimbursement program was labeled Meaningful Use in a top-down attempt to improve the way physicians use records.
EHR systems, unfortunately, can be habit-forming whether or not they provide the expected benefits. Institutions that adopt the systems soon find themselves locked in, their data having entered a cryptic format understood only by the vendor, so that data cannot be retrieved to move it to a different system. When the systems are ill-suited to modern habits (such as mobile access) or to new needs such as data sharing, institutions find a transition prohibitively expensive and disruptive.
So the US medical industry, under the guidance of the federal government, is taking on a huge collective risk: that EHRs promising Meaningful Use may fail to meet the new requirements, such as data exchange, during the day-to-day knocking about they receive (even if they are certified as Meaningful Use compliant). Thousands of new health practices adopting the EHRs would then join the earlier adopters as fellow prisoners.
Electronic record systems definitely improve safety in some ways—such as eliminating confusion in handwritten notes, and displaying warnings about adverse drug reactions—but can introduce other sources of error. The Institute of Medicine (IOM) issued a major report warning about safety problems in November 2011, the AHRQ prepared a report on tracking and assessing risks in electronic health systems in May 2012 (a summary of risks appears on page 29), and the Office of the National Coordinator, which is responsible for administering the government’s electronic health record program, released extensive safety guidelines in January 2014. Besides plain and simple bugs—for which vendors deny liability—problems include the following:
- Confusing interfaces that make it seem that some information was recorded when it was not, or the reverse.
- Arbitrary restrictions, such as drop-down menus, that leave out the medications or other choices that the clinician wants to make. Such counterproductive designs can tie up busy doctors and drive them to enter wrong data.
- Records that allow similar information in two or more places, thus creating such risks as duplicate doses. This can certainly happen with paper records too, but electronic records hide the duplication better and staff are less likely to know that duplicate locations exist.
- Information that is hard to see, perhaps simply because it is outside the visible part of the page and the clinician forgets to scroll the screen.
- Arbitrary decisions and defaults that are hard to discern and differ on each screen.
- Overuse of alerts. EHRs and hospital devices are programmed to react crudely to triggers, and manufacturers have set the triggers very sensitive for fear of missing something important. The result is that a doctor often cannot get through a write-up of a routine visit without clicking on innumerable dialog boxes to make them go away; for instance, some systems blindly report every possible side effect to using a medication. Clinicians get used to ignoring the alerts and ultimately might miss one that they really should have heeded.
Although EHRs theoretically allow doctors to customize the alerts that appear, no one has yet created a truly intelligent alert system with acceptable levels both of false negatives (which should be zero) and false positives (which are much too high now). Hospital wards are as noisy as tropical forests with the sound of beeps instead of animal calls. The constant din of multiple competing alerts creates a poor signal-to-noise ratio.
- Images that are distorted or have text overlaid in the wrong places.
- Unauthorized sharing of patient data, either intentionally or accidentally.
Like industrial accidents and airplane crashes, medical errors are generally emergent properties, caused by complex interactions of many factors such as haste, misreported symptoms, and plain bad luck. One factor is often an EHR that gets in the way, hides information behind multiple clicks, or presents a garbled display. Workarounds such as using sticky notes to store information before entering it in the EHR lead to more errors.
Errors in electronic records also tend to propagate. In such cases, one of the traits that makes them most valuable—data sharing—turns into a vulnerability. And a data breach with EHRs can put millions of patients at risk in one fell swoop, as front-page news reports regularly remind us.
The reporting requirements that the government and insurers pile on, potentially a boon for patient care and public health, create more work that is often redundant. For instance, stage 1 of Meaningful Use requires the doctor to report whether she checked the hemoglobin A1c of each diabetic patient. In theory, electronic systems should take on much of the clerical burden of such reporting requirements. The information that the patient has diabetes and that the lab ran a hemoglobin test is in the record, but current EHR systems do not automatically report it, requiring the doctor instead to do so manually. It would strike an observer as odd that such EHR systems could pass certification as Meaningful Use compliant, but neither the certification authorities nor the EHR vendors seem to care whether the doctor’s work is negatively impacted. No wonder doctors spend a third of their time with patients looking at a computer, imperiling their relationships with the patients (as we will see later, the core of medicine is the relationship).
There’s a movement among doctors for the FDA to regulate electronic records in hospitals as medical devices. Certainly, the agency has the tools to validate software quality for medical devices, looking at the development cycle, testing, and other external indicators of software quality. Nor is the FDA a stranger to software validation: it already regulates MDDS, which is a type of device that collects, stores, and transmits data from monitors and other medical devices, and has released principles of software validation. Requirements for EHRs might be along the lines of those used by NASA to certify critical aerospace software.
Proponents claim that similar regulation for electronic medical records, while increasing costs, will avert life-threatening problems. The most compelling argument against extending regulation to medical records is that the software would have to pass through the validation process after every change, slowing updates. But if a development process does not ensure quality, speed becomes a liability. A new paradigm for developing and customizing electronic records is probably more important than regulation. It might consist of the following:
- Intense clinician involvement in design
- The people using an interface must be part of the design team throughout the project, not just brought in as external consultants intermittently. Users who don’t understand IT can collaborate with IT professionals who don’t understand medicine to create effective tools, through iterative development and rapid prototyping. Some people say that the relative success of VistA sprang from its genesis among doctors and nurses at the Department of Veterans Affairs, who did much of their own coding. All institutions that are happy with their electronic systems have declared that the most crucial factor in their success was bringing in the staff and making them feel ownership of the transition. In fact, making a transition is so time-consuming that it probably exceeds the costs of the software.
Even after products are released, user interfaces must be easier to change. Electronic health records have some of the most notoriously user-unfriendly interfaces in the software industry. As mentioned earlier, the people making purchase decisions are usually in administrative positions. The dissatisfaction that doctors express about their record systems is legendary. Some of the complaints stem from clinicians that are not used to computers (yes, quite a lot of them are in the field), from the urgency and chaos endemic to many medical environments, or from resistance by staff toward relinquishing familiar workflows. But sometimes the record system imposes its own rigid workflow without just cause.
An AHRQ study on EHR usability laid out fairly simple requirements for tying patient information to treatment plans, but stressed the importance of selecting only the relevant information and presenting it clearly. Too often, neither EHR vendors nor internal IT departments understand what the physicians need to see and do not respect the value of their time. For instance, instructions for using software may be printed out as part of the patient’s record, probably by a programmer who couldn’t tell the difference between instructions and patient information. Such awkward interfaces drain precious time from the physicians’ and nurses’ days, reducing the time they can spend with patients and contributing to the serious shortage of physicians that threatens the hope for universally accessible health care in the United States.
- More agile systems
- Even though every health institution is unique and adapting electronic records to the enterprise is critical, most record systems offer very few customizations. It’s useful to allow doctors—as most record systems do—to choose which medications appear on a list of treatments for a particular condition, and which alerts pop up, but this is a far cry from making the software blend into the office’s workflow.
Serious changes to a product require an investment in certified consultants, additional paid contract work with vendors, or extra demands on overworked internal IT organizations that don’t possess the expertise to do the job. Changes that require vendor action take place on the vendor’s schedule. A common complaint among doctors is that new EHR vendors act responsive and agile with their first customers, and then turn just as blank and bureaucratic as all the older vendors when success and growth come.
When local sites do make customizations, they may be swept away by the next software upgrade. When smaller vendors go out of business or are merged into larger firms, maintenance and tech support may vanish.
- Better attention to safety
- EHR vendors contractually deny responsibility for errors entered into records through bugs or confusing interfaces. The health provider, who is presumably able to check for and catch any errors, bears liability for anything that goes wrong with a patient. To be fair, throughout the computer industry, software manufacturers commonly assert no warranty for software bugs. But the manufacturers should compensate by providing transparent, convenient feedback and tracking systems for bugs and product improvement suggestions.
- More transparency
- Contracts and vendor responsibilities could be much more balanced and reasonable, as recommended by the American Medical Informatics Association. This includes rights for software users as basic as discussing defects and the costs of products.
Some problems of EHR systems are solved at lower cost through free software. Free software or open source EHR systems include OpenMRS, Tolven, OSCAR, and several variants of VistA, whose development is now coordinated by a foundation called OSEHRA. VistA is gaining a bigger installed base, although its penetration is nowhere near what its fame would seem to deserve. The Open Health Tools consortium develops free software for clinical and research use. Deployments of open source health records in developing nations are supported by Partners in Health, among others.
The low adoption rate for these open source alternatives (at least in the United States) has been blamed on disparate issues ranging from sheer prejudice in the health care field to poor marketing. A good deal of this open source software originated in academia or government, and therefore isn’t backed by strong sales or support organizations. VistA’s dependency on MUMPS also dissuades enough potential developers that MUMPS wrappers have been created for other languages. But at base, the problem may simply be that an EHR system that truly makes life easy for clinicians has yet to be created.
It’s also possible that online, SaaS systems with essentially no administrative overhead are preempting any interest that might have gone to open source EHRs. But for reasons of security and accountability, it would be valuable even for the online systems to publish their source code.
One of the foundations of innovation consists of public data sets about providers, patients, and communities. But these public data sets join patients as victims of electronic record systems that capture data and don’t interoperate well. We’ll turn next to these data sets and what they offer.
Public Data Sets
Every year, the US Department of Health and Human Services holds a large national forum on health data. Dubbed a Health Datapalooza by the effusive Todd Park, former Department CTO, that name ultimately took hold as the official moniker. The forum highlights new data sets released by HHS and provides opportunities for activists as well as potential entrepreneurs to talk intimately to HHS and each other about uses to which they can put the data. This data then serves as a platform upon which state authorities can target high-risk areas, web sites can help patients choose health care providers, and other unanticipated value can arise.
HHS was not only one of the first institutions in the United States to offer open health data, but one of the first US agencies to join the open data movement, spearheading an open data gold rush on the federal level. Other countries offering health data include the United Kingdom and Brazil.
Public agencies gather huge amounts of valuable data, but its release to health providers may lag months behind the events tracked by the data. This can be blamed on the efforts needed to curate and clean that data, but also to bureaucracy, budgetary constraints, or workflows that persist from pre-Internet ways of sharing data.
Sometimes it may be hard to figure out what we can learn from the particular data being collected and released by governments, payers, or providers. But researchers from astronomers to military strategists have often had to draw on considerable cleverness to extract the insights they need from the data they can get. One example in health care is the use of data on referrals to infer the quality of doctors. Another example is a site that combines wait times reported by emergency rooms with traffic reports to suggest which emergency room will see a patient fastest.
Interesting public health benefits are emanating from organizations that manage to get their hands on data from lots of patients: services chosen by patients such as PatientsLikeMe and Web-based EHRs. By centralizing patient data, these companies can look for trends. For instance, when the 2013 federal government shutdown forced the Centers for Disease Control to stop tracking incidents of the flu, Athenahealth filled the gap. However, as we’ll see, privacy is better protected if patients store data instead of relying on either doctors or vendors.
Medical Coding Standards
Standards for entering diseases and patient conditions complicate clinical data entry. Both SNOMED and the ICD series are used to represent disease, but most billing in the United States requires ICD. Although the latest version, ICD-10, was finalized in 1990, and work on its successor ICD-11 is well underway, many US health organizations are still using the older ICD-9.
Based on assessments that ICD-10 will improve individual patient care, public health, and medical research, the government is now requiring a move to ICD-10 that is straining health organizations to a worrisome degree. ICD-9 was already hard to traverse, at 18,000 codes, but ICD-10 increases this number to 87,000 (see the Background section on this page). And ICD-10, developed as a reimbursement and billing tool, is hardly a perfect map of medical knowledge, especially with accelerating change from genomics, metabolomics, and systems biology. The American Medical Association labels the requirement to use ICD-10 as a distraction that will detract from the investments that physicians need to improve patient care.
Patients are variable. Not only are there many distinct medical conditions, but one condition will affect another. The designers of the ICD standards understood this and made a stab at representing relationships by extending the set. For instance, ICD-10 code Ill covers “Hypertensive heart and kidney disease” as well as “Hypertensive heart disease, w CHF.” The standard also tries to represent adverse effects of treatments through its T80 codes. But this is a game that could go on forever. A essentially flat, minimally hierarchical list of individual codes can’t possibly represent the complexity of interactions between medical conditions.
A superior way to approach intersecting diseases may be for a standard to represent diagnoses for individual diseases (at whatever level of detail researchers find useful) but create links between diseases, so that a doctor can indicate that one condition has caused, exacerbated, or hidden another. The Semantic Web is an example of how this can be done, and ontologies for ICD-10 already exist. Of course, representing relationships will still be a complicated task. We can only hope that tools for doctors and coders will emerge.
Reframing Clinical Research
Clinical research is the foundation of modern health—the rite through which new truths are revealed and verified—but even this hallowed institution is undergoing wrenching change. Researchers have been embarrassed by evidence that few scientific controlled experiments can be replicated, and that top publishers have been tricked into publishing computer-generated trash. Many shibboleths erected by clinical research in health care have been overturned through retrospective, longitudinal studies. Conflicts of interest also muddy the reliability of clinical research.
Additionally, big pharma is in trouble. Household names—Pfizer, Merck, Eli Lilly, Novartis, Bristol-Myers Squibb—who lavished billions of dollars on advertising, wooing doctors, sponsoring conferences, and lobbying officials are reaching the end of flush times. They have apparently already invented all the blockbusters—billion-dollar drugs that treat large numbers of people for common ailments—so they now need to invest increasing sums to find more elusive compounds serving smaller populations, and therefore generating smaller profit margins.
Compounding their distress is the expiration of patents that allow companies to enforce high prices through an effective monopoly on popular medications, and ever stricter requirements for clinical trials imposed by the FDA after disturbing safety lapses such the Vioxx case. For a number of reasons—some pertaining to FDA funding, but others springing from the difficulties of developing safe and effective drugs—http://bit.ly/1iF2iMM[the FDA is approving many fewer drugs than in the early 1990s]. Finally, researchers are having so much trouble getting patients in the US to sign up for clinical trials that a lack of subjects is cited as the reason behind the 40% of cancer trials that don’t run to completion.
Despite ongoing research efforts in genomics, biology, high-throughput screening, data analysis, and biotechnology, there have been no recent game-changing breakthroughs to unjam pharmaceutical progress, so companies are starting to look with a newly creative eye at clinical research. Innovations include:
- Looking for new incentives and means of outreach to increase the pool of patients willing to undergo trials.
- Using big data analytics to improve the targeting of diseases and the design of trials (including criteria for selecting participants), and using electronic records better to support trial operations, administration and data collection.
- Giving patients more of a say in the conduct of trials. Cracks are appearing in the research ivory tower through experiments in crowdsourcing, such as submitting drafts for clinical trials for public scrutiny, and even letting patients recommend what trials to run.
- Cooperating around basic research, called “pre-competitive” research, that precedes their efforts to produce a marketable result such as a drug compound.
- Releasing data from clinical trials, notably those trials that produce negative results most drug companies would rather not make public.
These all aim at a less top-down, more collaborative development process. A whole class of games such as Eterna engage the curious public to solve problems in genetics. Crowdsourcing sites such as Folding@home just ask for our space computer cycles, like SETI@Home famously does for astronomy. Merck is collaborating with a number of companies outside pharma, cognizant that its own medications and research concerning the larger aspects of disease management have to fit into an industry-wide scheme of data analysis, clinical care, and patient engagement.
Collaborative research requires data sharing, which in turn requires some agreement on formats and categorization of data. Sage Bionetworks is one of the organizations working on tools and standards for collaboration. A wide range of repositories, such as the Cancer Genome Atlas, offer fodder for researchers.
But data sharing can be a career-limiting move. Pharma companies risk that a competitor will build a patentable compound on top of their research and steal their market share. Lab scientists risk having someone else publish first (rival researchers have been known to win or lose publication races by a few days). Perhaps the health field needs to broaden its range of awards, so that a patent or published paper is not the gold standard for advancing careers and funding.
Meanwhile, a lot of people have decided not to wait for clinical trials, because they cost millions and can’t satisfy every question patients ask. The trials’ results often don’t even apply to many patients, because trial participants should be “ideal” subjects, healthy except for the condition the drug is meant to treat. Some patients are engaging in citizen science to host clinical trials or establish looser frameworks for discovering new cures.
Patients also come together through organizations such as PatientsLikeMe and 23andMe (which has had to suspend health-related activities after a dispute with the FDA over their claims) to upload personal genomics and disease information for data mining that can turn up trends long before clinical researchers could establish them formally. These health sites could be viewed as turbo-charged, data-driven upgrades to the forums that patients spontaneously form on social networks. They also represent a digital form of disease-specific patient alliances.
Barriers to Using Data
As the previous sections showed, data is everywhere, waiting to be used. Barriers to reaping its benefits include:
- Patient variability
- The intractable individuality of patients was one factor that doomed early expert systems. Nobody is a pure specimen of any single condition; everyone has complicating factors that require subtle weighings of possibilities. Therefore, no simple field on a chart or in an electronic record can capture every nuance of patient behavior. Diseases and conditions also interact, sometimes in nonobvious ways: for instance, knee injuries are related to obesity, while diabetes and urinary tract infections can exacerbate dementia. Complex histories are hard to record: a checkbox indicating whether or not a patient smokes can’t indicate whether he smoked for thirty years but successfully gave it up. Furthermore, computer systems can’t take into account that patients and doctors differ in their abilities to obtain, adhere to, pay for, deliver, and respond to treatments.
- Unstructured data
- Due partly to patient variability and partly to a long habitude of clinicians to use paper notes, an estimated 80% of medical data enters records as free-form text, along with images that also count as unstructured data. For most analytics, these records present a brick wall, although there have been recent advances in natural language processing for medical records. IBM’s Watson was already mentioned; other entrants in the space include Clinithink and Nuance. As an example of the difficulties such software must surmount, one can easily pick out the words “cocaine use,” but miss that the phrase occurred in the context, “cocaine use proven not to be a factor.”
Even if doctors enter data into structured fields, the EHR software may provide several different fields that could plausibly store the data, so the same information for different patients may occupy different places in the record.
- Privacy
- Many health practitioners claim that regulations raise barriers to useful data exchange, thereby holding back coordinated care. The heavy weight of regulation cannot be denied: in the United States we have the famous HIPAA law, continually augmented by hundreds of pages of interpretive regulations that change every few years, plus many state laws specifically dealing with health privacy. Small health providers complain that compliance places an outsized burden on them. But this is an area of much contentious debate, with many sophisticated clinical and IT leaders saying that HIPAA does not have to restrict useful data sharing and that it is simply misinterpreted by providers.
In fact, HIPAA has limited scope and fails to cover important privacy gaps. For instance, its “safe harbor” method of deidentifying patient data predates current advances in security and privacy protection, and thus is both woefully inadequate and unnecessarily restrictive. On the positive side, regulations were recently updated to ensure that business associates to whom health providers gave patient data had to comply with the law. Business associates are companies to which health provider outsource things such as billing and analytics, and who should not be taking advantage of the patient data given to them for such purposes.
Controversy exists over the collection of data from patients, even when it’s voluntary, because this data can be used for market research and other activities patients might not support. Because money spent to develop mobile apps cannot be recouped through sales, and because HIPAA does not cover apps (having been passed before the category existed), many developers collect and resell data from users. Patients also harbor quite reasonable fears, discussed under the section on public data sets, that a life insurance company, employer, or identity thief could deidentify the data and use it against the patient. Widely cited research by law professor Alan Westin shows that consumers worry about the safety of their patient data and want a say in where their data goes.
Public data sets may hold the secrets to improved medical treatment, but they are problematic from a privacy standpoint because it’s becoming easier and easier to identify patients who are supposed to be anonymous. Researcher Latanya Sweeney, who famously reidentified Massachusetts Governor William Weld from publicly available data in 1997, pulled off a similar feat in 2013 using health data from the state of Washington state. Data providers are improving their anonymization techniques, but they are fighting a constant battle against increasingly sophisticated data mining algorithms and the increasing availability of data sets on ordinary people.
- Conversion
- Organizations generally collect data in self-contained databases. A surprisingly large number still use flat files or spreadsheets. Although they could upload those spreadsheets and force users to download and disassemble them, data sets are more accessible when converted to a more computer-friendly format that allows simple programmatic querying. Converting data, as well as creating and maintaining future data in this way takes a big investment in many and IT expertise. It can’t be done just once, unless the enterprise adopts new technology, policies, and procedures to generate or incorporate data into the same system accessed by the API.
- Crushing standard compliance
- Health care systems usually have to recognize and produce data reflecting numerous standards. We’ll look at a few later in this section. The standards also change over time (although not as fast as the conditions they are trying to describe, leading to further frustration among physicians), which calls on the integrators and developers to absorb hundreds of pages of specifications for each new version and make sure the electronic systems comply.
A feasible solution to the patient record problem would involve:
- Free software
- A powerful open source EHR platform, widely adopted, could permit rapid innovation as new medical discoveries reveal the need for new data fields and interactions. Many projects larger than an EHR have been developed using free software methods, including Linux. It is noteworthy that most Linux development is now contributed by large corporations—Intel, IBM, Red Hat, Google, Samsung, and even Microsoft—who understand that investments in a robust, free software code base are paid back many-fold in the form of other business opportunities. Hospitals and governments have even greater incentives to support open source in health. Proprietary vendors, to reduce their own development costs, are getting more motivated to integrate with open-source solutions (e.g., via middleware).
- Application programming interfaces (APIs)
- Modern computing treats data sources as platforms on which other people can build applications. Cloud storage, with a standard interface into the data, allows innovators to flock to the underlying platform and enrich it through add-on software. RESTful APIs are quite flexible, have been popular for years, and are supported by powerful libraries in nearly every programming language. EHR vendors are finally starting to consider focusing electronic record systems on the backend tasks of data management, while turning themselves into platforms for others to provide user-friendly interfaces, workflow support, and analytics.
Promising initiatives come from the giant health plan Kaiser Permanente’s Interchange, from the payer/provider Aetna’s CarePass, and from the online record system athenahealth’s More Disruption Please. All of these institutions have offered platforms for third-party developers to develop applications based on their services.
- Analytics
- The data in electronic records needs to be useful if we expect it to be used. Its value comes largely from analytics that can extract trends from information about patients and the institutions treating them. Currently, “big data” (a convenient catch-all phrase for the enhanced statistical techniques now being used to explore correlations among large and often relatively unstructured data sets) is entering health care through numerous small companies wielding mind-numbing analytical expertise—expertise for which they compete fiercely, because the demand for data scientists is skyrocketing throughout industry, research, and government. But until basic analyses become cheap and universal, records in most institutions will still keep their secrets locked inside. Furthermore, health providers will have to realize that, in an environment of declining payments and of demands that providers show value for what they do, they urgently need these analytics.
- Patient control
- No one benefits as much as patients from the convenience and predictive power of electronic records. As we’ll see, patient control is not only feasible but a key to treatment and research.
Part of rethinking electronic health systems and their effects on the doctor/patient experience is to express the value of the digital systems to people entering all that data. Even if administrators and public health agencies get good data and analyze it to lower costs and improve population health—something that is barely starting yet—the doctors and patients who are interacting with the system will lack sympathy for those goals and experience nothing but the frustration and demands created by the system. Effective interaction requires a system design that benefits the end users, gets their consent for system use, and makes the benefits clear to them. This is all the more reason to open up electronic record systems and bring them into patient life—the goal of coordinated care, which we’ll look at next.
Coordinated Care: Teams and Telehealth
The current health doctrine—honored more often in words than in deeds—views people not as patients encountering the health care system through a set of discrete visits, but as full human beings needing lifelong attention. Indeed, this is the only way to treat chronic conditions, which are the health concerns of affluent nations. (As countries’ wealth increases, their health problems change from predominantly acute conditions such as infections to chronic conditions such as heart failure and diabetes, a shift called an “epidemiological transition.”) These conditions—lung cancer, liver cirrhosis, type 2 diabetes, cardiovascular disease—are also called “lifestyle” diseases. Now, there are plenty of chronic diseases that we don’t blame on the life choices of the victims—such as autoimmune disease—but these conditions still respond strongly to individual behavioral choices and need to be managed in people’s daily lives.
Therefore, researchers urge doctors to adopt a “systems perspective” in medical care. Viewing a patient as a system that constantly adapts to a changing environment can help a great deal in the long-term planning required for today’s chronic conditions. And the patient’s “system” includes not only her body, but her mental attitude, desires, and fears. Systems thinking also places a patient within a family and a community, which is crucial to effecting change. Living or working where lots of people smoke cigarettes, for instance, not only exposes a person to second-hand smoke but weakens his resolve to stay away from cigarettes.
Health care itself is also a system, as I mentioned at the start of this article. And it helps not only to view a clinic or hospital as a system, but to see the treatment team that surrounds each patient as one. Indeed, the patient’s relationship with a single physician is no longer enough. The physician must integrate tightly with other staff who deal with the patient—all the more since nowadays, given the doctor shortage, nurse practitioners and physician assistants do more in the sphere previously reserved for doctors. The system must also broaden to include the patient herself. Health IT tools can pull patient, physician, and other experts such as physical therapists, social workers, and nutritionists into a functioning team.
As a concrete example of the need for coordinated care, the preponderance of hospital readmissions come from nursing and long-term care facilities, and could probably be reduced by better exchanges of information.
Despite the increasing focus on chronic illness by health professionals, acute diseases still require prompt attention. The risk of epidemics grows with the concentration of people into large cities and their greater mobility, as a recent international initiative shows. That article mentions the use of motorcycles to report incidents. Digital technology can combine reports from individuals over mobile networks, data analysis, and coordination among health responders to deal with acute breakouts.
A consortium of providers trying to avert the need for hospital admissions have formalized patient/clinician relationships in the patient centered medical home (PCMH), which covers new options in treatment, monitoring, and reimbursement. Patient engagement in the home doesn’t require fancy technology: it could be achieved through follow-up phone calls and visits. But digital technologies can make the care less expensive and more responsive. The burden on both patients and caregivers can be lightened a great deal through technology, whether it’s simple reports by a patient via phone or sensors that track such things as whether she is moving around the house, how her weight changes each day, and whether she takes her medication.
Many PCMH initiatives depend on close human contact such as visiting nurses, with minimal technology. Simple things like card-holding sleeves can help patients and health workers coordinate their work.
Studies show that these innovations reduce hospital admissions for chronically ill patients, and particularly readmissions within 30 days after being discharged from a hospital, a measure that has excited hospital administrators ever since the Centers for Medicare & Medicaid Services (CMS) started in 2012 to penalize hospitals for such readmissions. On the other hand, like many health initiatives, the PCMH savings could get suctioned up by the bureaucratic costs for compliance and reporting.
Still, one would hope for better evidence than we have so far that this form of patient engagement improves outcomes. It may be that we don’t know what works yet, or are applying techniques inconsistently. Whatever we can do to keep patients in their homes will contribute considerably to improved quality of life and reduce costs by holding off their use of assisted care facilities. As we’ve seen, making the patient feel like an empowered partner, rather than a disparaged target of snooping, is key to success.
What comes after the PCMH? Naturally, the patient-centered medical neighborhood, which uses data about all patients in a clinician’s practice to draw conclusions about public health. This local use of data, however, just hints at the power released by integrating data across societies, a theme we’ll explore more under accountable care organizations.
Telehealth—a term I’ll use in preference to telemedicine, which evokes a narrower range of activities—allows experts anywhere in the world to weigh in on diagnosis. In many poor areas of the world lacking doctors, a patient can take a picture of a condition with a cell phone and send it to a doctor for evaluation. More commonly, a patient or doctor contacts the expert over an Internet video hook-up. Social networks among doctors, which allow them to share stories and ask for expert advice, may also fall under the umbrella of telehealth.
Now we need to consider some of the mechanics behind IT in health. One requirement—electronic data exchange—looms behind nearly all the advances being promoted: clinical research, patient empowerment, sensor data, telehealth, and more. The health field needs the same flexible, powerful capability for data exchange available to other organizations nowadays to carry out business and research collaborations. There is not much to learn from the data collected by any single hospital, so the institutions have to learn to create large, combined data sets. They also need to incorporate the data streams created by all the consumer devices described earlier.
Without data exchange:
- Sensors are mostly useless—they cannot forward their information to a central storage point.
- Clinical research is restricted to what a single lab can do on its own. This limitation is throttling modern pharmaceutical companies and academic researchers, who are running out of assets to carry out increasingly expensive trials on their own.
- Patient engagement shrivels, because patients cannot learn what their doctors know about them or share information among providers.
- Telehealth is blind, and becomes essentially impossible.
But the two technologies that permit electronic data exchange in most fields are crippled in the health care field. Only in the past year or two have breakthroughs been made, and they are far from being put in place across health providers:
- Formats
- In digital media, the format defines how bits are laid out so that someone can write a document on one side and someone else can read it on the other. In electronic health records, HL7 is the current state of the art in standards for representing patient records, but it does not provide unified formats; there are too many loopholes for putting data in odd places or defining proprietary fields. Furthermore, attempts to adapt to a semi-modern convention were done by translating a rather ill-structured older format of documents into XML, failing to produce valid XML and therefore leaving the documents hard to parse with standard XML tools.
The Consolidated-Clinical Document Architecture (C-CDA) in 2011 finally provided a more standard format supporting a wide range of clinical documents, and it was adopted as a requirement for supporting Meaningful Use. It is a complex format (taking up a 576-page draft specification) and still allows for proprietary extensions, a concession that is probably necessary to promote innovation.
- Exchange protocols
- In digital transmissions, protocols are the standards for opening and closing connections, authenticating and authorizing correspondents, and mechanisms needed to create and maintain communication. The first standard protocol defined in the health care field, CONNECT, began as a government effort as late as 2008 and uses complicated elements such as SAML (see the CONNECT site) and UDDI (see pages 12–13 of this PDF). Similarly complex SOAP technologies underlie the data exchange standard used by institutions to share health records.
Now the government is pulling the health care field behind two much more feasible standards, Direct for secure message exchange and DirectTrust for creating an infrastructure that validates the users on each side of the exchange. These do not guarantee, however, that doctors (and much less patients) can exchange records, because established organizations may block attempts at authentication.
Current standards have by no means solved the data exchange problem. The C-CDA is designed for the exchange of large documents, as the D in its name suggests. But as people collect data from devices and send them to doctors, they need protocols and formats appropriate for tiny, frequent transmissions. The creation of an an upcoming light-weight, RESTful protocol by HL7, the leading health standards body, is a major advance with much promise for opening up records, although it currently seems focused on conventional clinical information.
Security hangs over every development in the storage and exchange of patient data. While the Direct project focuses on email and the Web for secure data exchange, several commercial solutions try to solve the problem of sending secure messages among mobile devices, even “ephemeral messages” that get deleted after being viewed.
A robust electronic system would allow patients to share some parts of their records but not others—for instance, letting an orthopedist see records related to sports injuries but not mental health. This flexibility, known as data segmentation, has received wide endorsements in the field but also many criticisms, including from EHR vendors who decry the complexity it would add to their products and from physicians who are afraid they’ll be liable for data to which they were denied access. Still, support for segmentation appears in a major 2010 recommendation on health records by the President’s Council of Advisors on Science and Technology (see the section “Privacy Protection of Metadata-Tagged Data Elements” on pages 51–52 of the report).
Health Information Exchanges
The Internet permits any two sites using the same protocol to exchange data, a convenience we take advantage of hundreds of times a day. Why shouldn’t health data be exchanged just as easily? This is the goal of health information exchange (HIE), a term referring both to the act of sharing records and to institutions who exist solely to facilitate that exchange.
The security of sensitive patient data is a concern here. Drilled into anxious administrators by HIPAA and other laws, a concern for security has often been cited as an excuse for refusing to use HIE. But security shouldn’t be any more of a problem than it is for financial information or sensitive corporate secrets. Despite recurring security compromises, banking and industry depend on digital exchange. Indeed, clinicians use the Internet all the time for billing, the transmission of medical images, and other communications; it’s only treatment for patients that gets short shrift.
HIE has historically been tied up with expensive organizations that specialize in this area, which is like having to go to a special online broker to place your book order at Amazon.com. Because doctors had little incentive to give away the information they gathered about a patient, these organizations usually lasted only as long as a state agency, the US government, or some other outside funder was willing to pour millions of dollars into them. HIEs depended on proprietary software and offered little added value over a fax machine. Worst of all, they violated patient trust by selling data, taking advantage of a loophole in HIPAA. Recent efforts to rescue the concept still don’t promise long-term viability.
The very existence of HIEs was predicated on two problems: the difficulty of translating documents between formats, and the difficulty of matching patients. Each EHR vendor presented data in a different format, as we have seen. Thus, to serve hospitals using N different vendors, an HIE would either need N2 forms of translation software or develop its own internal format, along with 2N programs to translate their format to and from the format used by each vendor. A hospital may pay specialized vendors tens of millions of dollars just to integrate systems within its own institution.
The United States, unlike many countries, has no unique, universal identifier for residents. Although states are officially supposed to implement the REAL ID act of 2005 in their ID cards, public concerns over identity theft and surveillance have kept the government from enforcing the law. Therefore, clinicians and HIEs use up to 17 different identifiers (such as name, address, age, and birth date) to figure out whether a patient seen by one hospital is currently at another. A 153-page specification defines the Patient Demographic Query and Patient Identifier Cross-Reference standards that institutions use to ask about the presence of patients and make the match. Mistakes often lead to loss of life.
The US government is working on a voluntary identification system call Trusted Identities in Cyberspace (NSTIC), based on certificates not much different from those that validate websites, but the system is far from ready.
All this groaning infrastructure is a way to avoid a simple solution: leaving data in patient hands. The patient would just point a doctor to her online records before a visit. Professional services would crop up to help patients who don’t want to manage their own records. To cope with rare occasions when a patient is incoherent or unconscious (fears raised repeatedly by professionals opposed to patient control over data), patients could carry emergency phone numbers for relatives or other agents to whom they have granted access to their to records. Smartcards have also been proposed to hold critical patient information, or login information for their online records.
Recent changes in the field have led to slightly better prospects for HIE:
- The CONNECT and Direct protocols discussed in the section on data exchange, once they were supported by EHR vendors, allowed clinicians and HIEs to dispense with some of the complicated translation software they previously needed.
- Some HIEs realize they must provide more value than simply shuttling data between health care providers. These more forward-looking organizations typically provide patient stratification to their clients, using their knowledge of patient diagnoses to identify at-risk patients. These are the key contributions of the Beacon Communities set up by the government as testbeds for modern, coordinated care.
- Software vendors are providing various solutions to exchange and interoperability problems, often in middleware that an EHR vendor can use.
Yet despite these advances, few HIEs are surviving. It is time to remove them from the equation and use standards such as Direct to enable data exchange between doctor and patient, or between doctors under the control of the patient. Unable to get health information exchange universally available, payers are trying a different route to paying doctors for the value they provide, a principle known as accountable care.
Accountable Care Organizations and Other Integrated Care
Most developed countries take responsibility for their entire populations over long periods of time, and therefore have frameworks that potentially can handle (even if imperfectly implemented) integrated, long-term treatments of chronic conditions. Such health systems exist in the United States as well—the Department of Veterans Affairs and Kaiser Permanente, mentioned earlier, and the Indian Health Services—but most US residents get care episodically by doctors, hospitals, and insurers, who do not commit to long-term responsibility for the patient’s health or collect data over long periods of time.
The biggest upheaval in American health care in the 2010 decade may be the attempt by the Centers for Medicare & Medicaid Services (CMS) to reorganize hospitals and clinics into consortia with comprehensive responsibility for patients’ health. Called accountable care organizations, it encourages clinics and hospitals to combine and offer complete services to patients—in short, to act more like the Department of Veterans Affairs.
CMS encourages ACOs to reduce costs through incentives that work against the old toxic model of paying for each visit. Each patient in a certain category (such as certain types of heart disease) is assumed to cost a certain amount to treat. The ACO is rewarded for keeping costs below this threshold. The plan is a step toward global payments, which pay the health provider a fixed sum to take care of a defined population.
The payment and policy issues created by this situation lie beyond the scope of this article, but we can certainly look at the IT that would be required by an integrated health system.
Determining how much a particular patient should “cost” is a difficult judgment that requires better data than we have now. Furthermore, the three-year period for which an ACO is considered responsible for a patient may not be long enough to see improvements in chronic conditions. But the problems with ACOs go deeper.
Few ACOs have been set up yet. CMS presents early evidence that ACOs are saving money, probably by picking off the low-hanging fruit. (Without technological razzle-dazzle, Blue Cross Blue Shield also announced significant cost savings from value-based care.) A successful ACO meets the “triple aim” in health care—improving the patient experience, achieving better health, and lowering costs—through such data-rich activities as:
- Tracking the patient from primary care to specialist to hospital to physical therapist and so on, making sure the patient follows up on recommended treatments.
- Sharing a patient’s records expeditiously among all the clinicians working with the patient.
- Crunching data about patient conditions and outcomes to find where treatments succeed or fail.
- Using this longitudinal data to predict trends, which could help apportion resources more efficiently and even contributes to public health.
In the best case, fixed payments and rigorously monitored outcomes—both are necessary to make the ACO work—will inspire providers to look for efficiencies.
The activities just listed show that, essentially, to be successful, an ACO has to exchange data seamlessly as the patient moves through its system. Three elements have been identified to summarize ACO needs: analytics, workflow, and communication, all of which depend on an integrated health IT system. One might think of ACOs as bringing health information exchange within the boundaries of the cooperating providers. As we have seen, current EHR systems are not capable of seamless exchange.
ACOs are also at constant risk because a patient has the right to get care from someone outside the ACO. They need powerful incentives to keep each patient within their system.
Applying scrutiny to the needs and problems faced by ACOs reveals that these problems are best solved on a more global level; most individual ACOs lacks the wherewithal to solve it themselves. In particular:
- Data exchange requires robust, easy-to-implement standards that should be reached at a national or even international level. To glom together local hospitals and clinics into ACO and expect them to harmonize their record systems is too much to ask. The problems of current ACOs show how integration through data sharing is both critical and hard for them to achieve.
- Decision support and public health are facilitated by huge data sets. The more institutions combine to exchange data, the more they can learn. As we shall see, a national public health plan could be built on data stored by patients and shared at their discretion. Although some individual hospitals have learned valuable lessons by tracking their own data, and Kaiser Permanente has achieved a lot by exploiting its huge size, a national health system would generate far better data than the amount an ACO can collect.
A perennial complaint of health reformers has been the isolation of data and decision making by individual doctors and institutions—data silos, as they are called. ACOs just create bigger silos needing standards for data sharing and interoperability. The system seems to be an attempt to ward off the solutions that would enable health information exchange throughout the health care system.
ACOs also risk raising costs by creating larger, more powerful players, a risk CMS is apparently willing to take in the hope that better coordination in the long run will lower costs. I consider ACOs an experiment whose lessons can be eventually applied in a national plan for data exchange and coordinated care.
Telehealth
This buzzword has been applied broadly to many aspects of health care. Examples include the following:
- Contacts by phone or text messages to remind patients of basic treatments, such as coming to doctor’s appointments or taking their medications. Rudimentary technologies can be used in very sophisticated ways. For instance, recruiting a family member to text a patient may produce a better outcome than receiving an impersonal text message from the clinic. Prevent goes even farther, linking people at risk for diabetes with coaches and other participants over a mobile device.
- Remote consultations. These may take place between a patient and a doctor, or between a doctor and a specialist. Although the use of video connections for mental health treatment was disparaged for a long time, many patients find it helpful.
- Contacts with patients in their own homes, discussed earlier.
- The high end of telehealth is the remote monitoring of ICU patients, which sounds sub-optimal but can actually do better by patients than depending on staff in the unit. Intensive care units are laden with sensors, which can be monitored by experts outside the center just as easily as by nurses on the floor. Technology now also allows remote monitoring of trauma patients while they’re being brought in from the scene of the trauma.
Remote medicine changes the health equation for people living in areas underserved by doctors, such as rural areas and developing nations. Ordinary residents of poor areas, even children, can be taught to run phone apps that walk them through questions to help determine what is wrong with a patient. They can also take photos of afflicted areas of the body and send them to doctors in cities better served by clinics. One example is a modified mobile phone that can take pictures of the eye.
Many applications of telemedicine simply extend the reach of a doctor, not much different from placing a telephone call. These applications conform to a traditional model of health care, albeit with some convenience for the patient and notable cost savings. But truly transformative telehealth involves a large set of the technologies we have examined for collecting, exchanging, and analyzing data.
Payment models need to change drastically to accommodate telehealth. Currently, most payers won’t even reimburse a doctor for using email or the telephone to advise a patient instead of a visit to the office. But many states are preparing legislation to allow telemedicine, and a bill introduced into Congress would promote consultations with doctors over state lines. Because doctors are comfortable initiating consultations and patients in underserved areas crave contact with professionals, telehealth should become very popular once the enabling factors are in place.
Barriers to Coordinated Care
The main barriers to data exchange are institutional decisions. Hospital and clinic administrators know that making data portable will ease the way for patients to find other providers, should they choose to do so. ACOs, like bilateral or regional trade treaties, are formed to preserve competitive advantages over outsiders. EHR vendors undermine interoperable standards (to the point of lobbying on relevant legislation and regulation) for the sake of their clients as well as to preserve barriers to entry in their own markets. Pharmaceutical companies and clinical researchers guard secrets to further their careers. And even though HIPAA requires data sharing, health providers like to claim that they can’t release data because of HIPAA.
But even accounting for all those considerations, we also have to acknowledge technical barriers to health information exchange and, consequently, to coordinated care:
- As explained under barriers to using data, people are inherently variable, so data exchange could be comparing apples to oranges.
- Data collected by researchers is just as variable as data from medical records. One researcher will collect data under different temperatures or other conditions from a researcher next door, or divide the data into different categories.
- Errors are rife in medical records, whether on paper or in the computer. It has been estimated that everybody’s record has errors. (Try reading one person’s account, plus some of the comments.) These weaken the validity of conclusions reached through data processing. Statisticians and data scientists have developed algorithms to compensate for suspicious data fields, which makes the data more usable in the aggregate. But algorithms don’t actually correct the data, which needs the patient’s eye.
- Good equipment for telehealth can be expensive. Bandwidth for video hook-ups, for instance, is not universally available. And although an image may be sent to a clinician’s cell phone, the phone’s screen probably lacks sufficient resolution to show the necessary detail.
- Clinicians resent the time taken up by reporting requirements, such as checking hemoglobin A1c for diabetic patients. A tension will probably always exist between offering immediate treatment for a patient in the office and providing statistics for valuable longitudinal analytics. Technology should reduce some of that tension by automatically extracting the necessary reports and verifying their accuracy.
- Segmentation may turn out to be a mirage, even if the considerable technical hurdles are overcome. For instance, if a patient asked the doctor to segment his diagnosis and treatment for an STD, the doctor would have to properly tag everything from the clinical interview and the lab test to the diagnostic code and the medication assigned. It’s too easy for a lab test or medication list to give away the truth, even if a diagnosis is hidden.
Patient Empowerment
Everything we’ve seen in health IT advances so far point to a bigger role for individuals in their own health care. Health experts like to talk about “patient engagement” or “patient satisfaction,” condescending terms that suggest the doctor has all the answers but needs to make stupid or recalcitrant patients comply. Patient advocates prefer the term “patient empowerment” and replace “compliance” with “adherence.” The very term “patient,” reeking of passivity and helplessness, irks some advocates, but other terms such as “consumer” have problems too.
The psychological, organizational, and policy implications of patient empowerment (or even engagement) are huge, but this article focuses on the role of computing and data. How can health IT help move care to its new locus, the individual? We have already discussed patient-centered medical homes, Quantified Self, and openings in clinical research, but less obvious changes can suffuse patient empowerment through the health care field.
Health Care Without a Doctor
Insensitive doctors sometimes act as if the patient was not a factor. People are turning the tables now, engaging in many health-related activities without involving clinicians. And today’s technology is replete with playthings and baubles for the motivated individual—often acting in collaboration with peers. The technologies can bring real benefits.
For instance, a number of mobile apps help veterans manage stress and mood, while several apps such as STOMP offer regular encouragement to tobacco smokers who want to quit. Games improving brain performance are a particularly popular niche. Sites such as OneHealth and Helius are broader and more strategic, setting up plans for patients to follow in their daily lives.
People often use social networking sites with which they are already familiar, such as Facebook, to form communities around health issues. Others choose specialized sites such as PatientsLikeMe. People can even share test results with potential sexual partners to provide assurances that they are free of STDs.
The entrenched conservatism of the health care industry have driven many, such as the illustrious chronicler of “disruptive innovation,” Clayton Christensen, to suggest that change will be forced on the health care industry from outside. These reformers will celebrate as the metaphorical countryside advances on the city. But disruption is not a total solution, because someone must still provide the knee surgeries, the colonoscopies, and the other major procedures and tests that more and more of us demand. And disruption cannot ignore the imperative of coordinating long-range individual behavior. Perhaps outside organizations can disrupt health care, but only if they move beyond “urgent care” or walk-in clinics to care for the whole person over a period spanning decades.
Gamification
One exciting area of health research is the use of video games. All types of games can be impressed into service in the pursuit of better health: mental challenges, role-playing games (for clinicians as well as for patients), competitions, and even the old stand-by: first-person shooter games.
A game is an automated form of patient engagement, along the lines of text messages reminding them to take their medication, but infinitely more powerful. No one has to ask a patient to be engaged; with a game, he chooses to be so.
It may not be surprising that games can ameliorate mental conditions such as Attention Deficit Disorder or Post-Traumatic Stress Syndrome. Perhaps more thought-provoking is their role in helping stroke victims and cancer patients recover. The combination of games and devices creates a whole new playing field for medical research. For some people, games outperform medications in every way, proving in some conditions to be cheaper, more effective, less dangerous, longer-lasting in their effects—and, of course, more fun.
Why do people love games? Several explanations have been raised, including the story-telling suggested by a game and the way it makes people feel they’re in control. The feeling of control is a bit odd, because every detail presented to them on the screen—assuming it’s a video game—has been planned and programmed. In any case, games feel like the ultimate in putting the patient in control. Games also make maximum use of feedback loops, which people use in all areas of life (and health) to encourage positive thinking and behavior.
Finally, many games are social. One can compete with others for achievements and at the same time feel spurred on by their support and cameraderie to make behavior changes.
Transparency
Economists and other observers of the health care industry have understood as far back as 1963 that it is not a true market. Many wish that it was one—a level playing field where patients knew the costs of care, the quality of the provider, and all their options. But in the United States, all too often:
- Not even the provider knows how much a patient will pay until the insurance payer issues a statement, often after the procedure has taken place. Prices are set in secret negotiations between providers and insurers and vary among patients.
- Hospitals conceal the rate of complications, rehospitalizations, and deaths from procedures, and even though governments often collect such information, they rarely publicize it so that patients can compare doctors. Reputation is a poor guide to actual quality. To top off the problem, patient ratings are mostly irrelevant, being based more on the quality of the food or the amount of noise in the corridor (not that these are unimportant) than the success or failure of procedures.
- Physicians try to present alternative treatments (including the alternative of no treatment) to patients, but it’s hard to predict the relative success of each treatment. Genetic analysis can often indicate what will work for a particular patient. Many new treatments come along that doctors aren’t aware of. The success rate of more experimental treatments may be unknown.
Governments have started releasing data about hospital quality, and some intrepid sites such as Clear Health Costs use public data sets and crowdsourcing to build support for patients trying to compare costs. Castlight includes health cost and quality measures as part of a service to employers. Pressure is rising for more price reporting.
Observers have worried that making prices public will actually lead some facilities to raise prices. But when the day comes that everyone can see the price and outcome of popular procedures, the market will take over and crush institutions guilty of bad care or overcharging. Posting prices clearly might also cut down on some of the fraud that officials guess adds up to thirty billion dollars or more per year.
Patient Control Over Data
What have we seen about patients in our tour through modern health care in this article? That patients can benefit from the output of sensors and monitoring, which is by definition their own data. That electronic records are the basis of better care, but are most secure and available when the patient has control over them. When you think about it, patient empowerment is meaningless without patient control over data.
As mentioned earlier, doctors routinely ignore the legal requirement to show patients their health records. Institutions affiliated with OpenNotes offer patients ready access to all their data (including their doctors’ notes) through patient portals. They found that this provides several clinically important advantages. For instance, patients report taking their prescribed medications more often. But patient portals remain clunky at best. While they are evolving rapidly, they’re still a long way from being as empowering as records that patients maintain themselves.
Two major projects have offered patients a place to keep their own health records: Google Health and Microsoft HealthVault. Google closed its service because it wasn’t taking off, and adopters of HealthVault are also fairly sparse. Many explanations for these lackluster results have circulated. Some claim the services were difficult to use or lacked important features, some cited a lack of appeal to patients (including worries about breaches of privacy), and some noted resistance put up by physicians, providers, and payers, who feel threatened by patient-owned data and want control for their own financial benefit. In any case, it’s clear something big has to change to give patients their damn data (video).
One feature of the winning electronic health system is sure to be free software, which already offers several promising developments:
- Indivo to store data
- An inspiration for Google Health and an actual source of some of HealthVault’s source code, Indivo is a free software personal health record. It includes an API to let other EHRs upload data to it—but no simple way to download data in bulk, because the developers’ goal is leave data under the patient’s control.
- Blue Button to download data from EHRs
- This project, the brainchild of the Department of Veterans Affairs, has become a standard for the whole health industry. When Blue Button started, the project was simplicity itself: a patient could press a button on the health provider’s website and receive a down-and-dirty, plain text list of his conditions, treatments, and other facts. A more structured XML format has now been developed to make the data friendlier for apps as well as human readers, and it’s eminently usable for OpenNotes.
- Direct for data exchange
- Introduced in the data exchange section of this article, Direct makes secure exchange of patient data possible even if both sides have nothing more sophisticated than email. Because encrypted email is so rare, most users will have to contract with a website to protect the transmission, but the website already plays a key role by authenticating the person with whom they want to exchange data.
Health providers are gradually putting data in the cloud to reduce costs, improve security, and make access easier, so there is no reason the records shouldn’t be under the control of the patient instead of the provider. Smartcards, which have been used in France and other countries for many years, may also work in tandem with personal health records, making it easy for patients to bring their data to many health providers.
But even if someone weaves all these technologies into an appealing and usable patient record, how can patients be encouraged to use the records, and doctors encouraged to consult them? The key to progress returns, perhaps, to the very first element of health reform listed in this article: sensors worn by patients to preserve their observations of daily living. Such data could grow in value to become indispensable, whereupon doctors and their EHRs will have to open up to patient-maintained records.
Several leading health IT groups have asked the Department of Health and Human Services to require health providers to accept patient data in Stage 3 of Meaningful Use. But because consumer devices report their results to data silos maintained by the device’s vendor, the patient must also be able to run a simple program to capture the data, either from the device or from the vendor’s site.
When patients insert data into records, encoding them with a provenance becomes even more important. It’s always valuable to know how data was obtained, but doctors are particularly cautious about measurements that were taken outside the clinical setting.
Patients have been advocating for access to their records for many decades, but technology is finally emerging to back up their demands. This article has hopefully suggested some of the significant advances that the health care field can make when their demands are met.
General Closing Thoughts
It’s no coincidence that President Obama—along with many other presidents from Harry Truman through Bill Clinton—made health care reform central to his administration. Americans are facing multiple health crises, whether from the effects of obesity or the tragedy of drug addiction. Health costs are bankrupting the nation—when people talk about the federal deficit, they are largely referring to Medicare’s expected payouts. And Americans are just plain terrified by the prospect of getting sick and not being able to get treatment.
And although the United States spends far more than other nations for health, without commensurate outcomes, the problems are not limited to this country. The ratio of elderly to working-age people throughout the world is increasing as their incomes and life opportunities expand, while breakthroughs in treatments raise expectations for care.
Caution among payers, providers, and administrators toward disruptive innovation is understandable. People can get hurt if something goes wrong, and decades of fail-safe practices to protect patients have been built up that put a damper on experimentation.
It is not within the scope of this article to discuss health care policy. As for fears that the Affordable Care Act will raise costs, I’ll simply say—if you provide people with health insurance but don’t actually make them healthier, no doubt costs will go up.
Thus, regardless of the fate of the ACA or of political controversies, it is critical for societies to make use of available data and computer technologies. Patients must get their data and must be encouraged to provide it to researchers. Analytics must be made widely available and used sensitively to reveal the places where health care can improve. The improvements may be as simple as a reminder phone call, as sophisticated as the identification of hot-spot neighborhoods, or as dazzling as the discovery of new miracle drugs. Technology and social change will meld to create medical progress, regardless of any hype or overinvestment that may be taking place in the early 2010 decade.
People in hi-tech like to lecture the health care field to adopt more of a “Silican Valley mentality” (this example is typical, although Amazon.com is not physically located in the Silicon Valley). While the meaning of that phrase is vague, it usually brings to mind young hackers making prototypes and rolling out rapid updates, funded by open-handed venture capitalists (at least until financial bubbles burst). But in my view, these activities are not the most important aspects of success in the Silicon Valley. Furthermore, the modus operandi is not appropriate for health. In health, the consequences of a bug are not just a message informing a visitor she cannot post a photo. It could mean that a patient is missing urgent treatment, or being given too much radiation.
The true energy behind the “Silican Valley mentality” lies in the inquisitive people meeting nightly in basements, kitchens, and hacker spaces all over the region to show what they’ve been doing lately, discuss problems, and come up together with solutions. This mentality is not taking hold in health IT. User groups meet for various products, but everyone overall—hospitals, researchers, EHR consultants—is trying to preserve secrets and use other people’s ignorance to their competitive advantage. Only in hackathons can one find an open attitude toward making progress. Until health IT experts form communities to discuss what’s bothering them and seek common ground, there will be little of the Silicon Valley mentality in health care—and little reform either.
In a health care field dominated by chronic illness, health lies in the hands of each of us. But we can’t get better unless we work together. Sensors, data, personal health records, data sharing, and open source software are all part of that collaboration.
I’d like to express my appreciation to the many people who reviewed and supplied ideas for this article, including Marie Dunn, Tom Delbanco MD, Bonnie Feldman MD, Adrian Gropper MD, Ellen Martin, Scott Monteith MD, Nate Osit, John Reddick, Shahid Shah, Scot Silverstein MD, Fred Trotter, and John Wilbanks. I take responsibility for all facts and opinions stated in the article.
