Tiny components can have huge effects. Even if you’re not a weather scientist who embraces Chaos Theory (the flutter of a butterfly’s wings in Mexico changes weather patterns in America), you know a computer chip the size of a fingertip can contain millions of invisible gates, and the loss of that chip means that the seven-million-pixel Photoshop montage you’ve been working on for that DVD cover just vanished forever.
A seemingly innocuous glitch can bring down software programs comprising hundreds of thousands of code lines. Ever heard of that impossible-to-find “divide by zero” bug? Just because something is small doesn’t mean that its influence isn’t giant. Such is the case with the micronutrients in our diet.
“Vitamins schmitamins,” you might say.
All you have to know is that the continuous deprivation of really tiny amounts of vitamins B1 (thiamine) and B3 (niacin) can give you nasty, potentially fatal diseases called beriberi and pellagra, respectively. These diseases have been very common throughout human history.1 And these vitamins are recommended only in the micrograms per day.2
If your dinner was a beach, the B vitamins would be a palmful of sand.
What about vitamin C, which has been urged upon you ever since that apple banged around in active competition with the Twinkie inside your lunchbox?
According to a 2004 study that tested thousands of Americans for their health status, up to 3 in 10 Americans have either a deficient (about 7 percent of them) or marginal vitamin C status, meaning that if the C starvation continues, they could be a few months away from real scurvy symptoms3 (see the sidebar Vitamin C: Helps Keep Your Tissues and Fat-Burning Capabilities Intact).
Note
Full-blown scurvy is a potentially fatal and ghastly disease, involving bleeding from ruptured blood vessels, as well as the overall disintegration of collagen, the fibrous, bodily connective tissue found in tendons, ligaments, cartilage, skin, bone, muscles, and veins. Vitamin C must be present for the synthesis of collagen, which is why you literally fall apart without it!
Now that I’ve mentioned it, a medium-sized apple contains about 8.4 mg of vitamin C (you need on average about 6 mg of vitamin C per day to avoid death!), so you need to go quite a bit farther than the apple to reach the RDA of 90 mg for men and 75 mg for women.
The good news is that it’s generally very easy for the vast majority of people to get enough micronutrients via their diet alone (if you make the effort to educate yourself on food composition), or through a combination of food and supplements.
You have to derive micronutrients from your diet and/or supplements, because the body cannot make most of them itself. In fact, we’ve evolved a love affair with plants due to that age-old drawback of not being able to synthesize life-giving chemicals like vitamin C or E as plants can (see the sidebars on vitamin C and antioxidants).
You might recall this story: the British sailors keeled over with scurvy, but the cats on the ships survived, because they could synthesize their own vitamin C (thus the “Limeys” began eating fruit like vitamin C–containing lemons and limes to survive sea voyages).
People have a small but crucial requirement for vitamins or minerals in their food. An upcoming section explains the daily requirements for micronutrients, which the Food and Nutrition Board of the U.S. National Academy of Sciences establishes and calls Recommended Dietary Allowances, or RDAs.
Sometimes a doctor, or a friend, or the local guru who seems to have read every Asian philosopher and can walk anywhere barefoot, scratches his chin and says something like, “Maybe you should take more magnesium. . .”
Because it’s generally to your advantage to be able to distinguish magnesium from vitamin C (for beginners, one’s a mineral and the other is a vitamin), this chapter will also provide brief descriptions of many of the key vitamins and minerals.
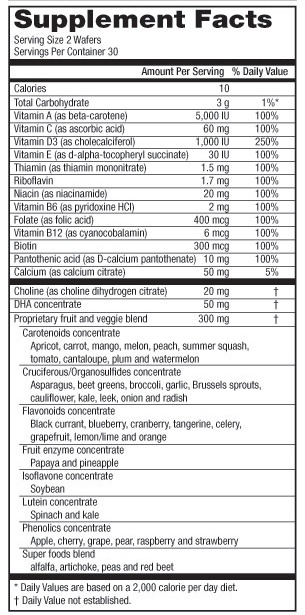
Along the way, the chapter gives you tips on reading a vitamin Supplement Facts label, as well as sensible reasons to aim for some of the “super foods” like the tiny but mighty phytochemicals.
The end of the chapter has a guide to a few of the online tools you can play with for analyzing your nutrient intake. After all, knowledge is power, especially self-knowledge. Your nutrient profile might begin as a sad story, but it’s going to end in triumph.
Let’s get some definitions out of the way first.
A micronutrient is a tiny constituent of food or a biochemical that plays a vital role in basic physiology, such as a vitamin, a mineral, or a phytochemical—that is, a chemical made by plants, such as beta-carotene, lycopene (in tomatoes), or resveratrol (in grapes).
Macronutrients (discussed in Chapter 3) are the dietary components used for fuel and making things, and are thereby used up in the process: protein, carbohydrates, and fats. Micronutrients are used for chemical reactions (vitamins can be cofactors for enzymes) and/or stored in the body as part of its structure or chemistry (e.g., calcium and phosphorus in bone), or as antioxidant defenses (vitamins C, E, and the mineral selenium).
Micronutrients are often measured in milligrams or micrograms. There are about 28 grams in one ounce; a single U.S. dollar bill weighs about 1 gram. A milligram (mg) is one thousandth of a gram. A microgram (mcg) is about one millionth of a gram.
Sodium chloride (salt), for example, is a “macromineral” that people eating Western diets typically get more than enough of from processed foods. A macromineral is usually required in the diet at a quantity of at least 100 mg or more per day, but all of our descriptions will mention specific RDAs along the way.
To picture a milligram, imagine one grain of salt out of a saltshaker. Some of the trace or “microminerals” we list in this chapter, like iodine or selenium, along with B vitamins, for example, are only recommended in a few mg per day, or in some cases, a few micrograms.
As in the user-testing and bug-tracking tools of the software world, you have to have some kind of metric to determine whether you’re getting enough of a micronutrient or not. You may know you’re getting 50 mg of vitamin C per day, but then what? Is that too much, not enough, or adequate for your age or gender?
In the U.S., the Food and Nutrition Board of the National Academy of Sciences has set the daily requirements for vitamins and minerals. They call them Recommended Dietary Allowances (RDAs), and they are usually expressed in milligrams or micrograms. The RDAs are the amounts of the chemicals that will keep you out of deficiency for that vitamin or mineral (meaning, they are not maximum intakes by any means). They are part of a larger rubric called Dietary Reference Intakes, or DRIs (see the end of this section for an explanation of the “dietary alphabet soup”).
Some of the vitamin recommendations are in International Units (IU), such as for vitamins A and D.
Note
To convert from IUs to micrograms, for vitamin D: 1 IU = 0.025 mcg (so 40 IU vitamin D = 1 mcg). For vitamin A: 1 microgram = 3.33 IUs.
An RDA is pretty easy to understand: for example, 90 mg of vitamin C for male adults and 75 mg per day for female adults.
The RDAs are not generally hard to meet by eating whole foods such as fruits and vegetables, but that hasn’t prevented the vast majority of Americans—more than 90 percent of us—from falling short of the requirements, according to Dr. Jeffrey Blumberg, the director of the Antioxidants Research Laboratory at Tufts’ Jean Mayer USDA Human Nutrition Research Center on Aging.
A multivitamin is “insurance” against being deficient in vitamins and minerals, he said, but not a substitute for healthy foods. Eating healthfully versus taking supplements is a “false dichotomy.”
The vast majority of people need to do both, but you shouldn’t view supplements as taking the place of fresh plant foods, which, unlike your multivitamin-mineral (MVM) supplement, contain dozens of important phytochemicals like beta-carotene, lycopene, flavonoids, and epicatechin (in green tea).
Note
Some newer supplements are jammed with a lot of “super ingredients,” but these products are unregulated and may be fraught with uncertainty. You might as well graze the farmer’s markets and stands for fresh sources of flavonoids and other phytochemicals, because these appear to be roughly the types of nutrient sources that humans have sought throughout our evolution.
We probably evolved to graze on plant foods and thus inherit their protective antioxidant and anti-inflammatory defenses (see the sidebar Antioxidants: Cultivate Your Inner Nerf). “We lost the ability a long time ago, when we became human, to synthesize these compounds [internally] ourselves,” Blumberg said.
That’s all you really have to know about RDAs; they are not a maximum amount for your intake, but rather the minimum amount required to keep you from becoming deficient (the upper limit is abbreviated as TUL). For what it’s worth, the overall DRI is explained here: http://www.ars.usda.gov/News/docs.htm?docid=10870.
According to this site, the DRI’s are actually a set of four reference values (of which RDAs are one).
“Recommended Dietary Allowance (RDA) is the average daily dietary intake of a nutrient that is sufficient to meet the requirement of nearly all (97-98%) healthy persons.
Adequate Intake (AI) for a nutrient is [...] only established when an RDA cannot be determined. Therefore a nutrient either has an RDA or an AI. The AI is based on observed intakes of the nutrient by a group of healthy persons.
Tolerable Upper Intake Level (TUL) is the highest daily intake of a nutrient that is likely to pose no risks of toxicity for almost all individuals. As intake above the UL increases, risk increases.
Estimated Average Requirement (EAR) is the amount of a nutrient that is estimated to meet the requirement of half of all healthy individuals in the population.
Taking a multivitamin/mineral supplement is about half (or less) of the picture of micronutrients. The other half is the fun part: eating for health.
I try to aim for foods from local farms and farmer’s markets (see Chapter 5, for more on finding and choosing food). I seek to get most of my vitamins and minerals from healthy foods. By targeting healthy foods, I mean piling on the veggies (carrots, lettuce, yellow/red/orange bell peppers, broccoli, asparagus, etc.) and fruits (lots of berries, fresh apples, oranges, bananas, lemons), as well as eating pastured dairy (butter, cheese, milk), coconut milk, grass-fed meats, fish (including shellfish), a fairly neutral grain like brown rice (grains can be problematic), as well as some nuts, seeds, and plant oils like a little olive and coconut oil.
The tools we discuss at the end of this chapter will help you determine whether your vitamin and mineral consumption is adequate or not. The degrading of nutrients in kept food is an issue, too. Oxidative damage (think juice in paper cartons, or old refrigerated veggies that have changed in color) can degrade a food item’s nutritional content, and supplements whose expiration dates have passed will no longer have the potency indicated on the bottle.
Note
Use common sense: a ready-to-drink carton of OJ may quickly lose its vitamin C content in the refrigerator (using glass containers and drinking it fresh from frozen are better), according to Professor Carol Johnston at Arizona State University. Gnarly-looking veggies orphaned in the back of the food drawer have probably also lost a lot of their antioxidant and vitamin power. Check the expiration date of any multivitamin/mineral supplements (MVMs).
For most of us, life involves a marathon of over-programming and scheduling that keeps us sitting down most of the time and snatching random food items here and there on the run. As a result, some of us might benefit from a multivitamin/mineral supplement, but a healthy dose of skepticism in regard to the quality and efficacy of these products is in order.
The bioavailability of these artificially manufactured nutrients is a highly significant variable as well, according to a 2006 executive summary in the American Journal of Clinical Nutrition.4 Here’s their take on this issue:
Key factors determining the bioavailability of micronutrients are the chemical form in which the nutrient is presented to the intestinal absorptive surface, the presence of other competing chemicals in the intestinal lumen, the concentration of food constituents (such as phytates and other chelating agents) that bind to the nutrient and make it unavailable for absorption, intestinal transit time, and enzyme activity.
A nutrient may affect not only the absorption of other nutrients, but also the transport, tissue uptake, function and metabolism of other nutrients.
Note
The following URL, a search of Google Scholar, provides much food for thought on the matter of nutrition in a pill: http://scholar.google.com/scholar?q=efficacy+of+multivitamin+mineral+products&hl=en&btnG=Search&as_sdt=1%2C46&as_sdtp=on.
We can probably benefit from a measure of insurance. You might mix and match a supplement (e.g., D3, calcium, magnesium) with healthy foods from local farms in season. If you are a nutrition power user, and I’m guessing many of the readers are, you could actually test yourself for vitamin and mineral insufficiencies before committing to certain MVMs and nutrient intakes.
I recently spent the better part of three days climbing Mt. Rainier, a 14,411 ft. active volcano near Seattle, Washington. Nothing grows up there. All water comes from melted snow. The food the guides cooked in the mess tent was outstanding in taste (veggie burritos loaded with avocados and tomatoes, gorpy oatmeal, and mounds of cheesy eggs and bacon), but I couldn’t have lived on it 100 percent of the time, in terms of micronutrient intake. Obviously, if I were spending weeks on a mountaineering trek in similar environs, I would consider bringing a vitamin and mineral supplement to buoy up my nutrition.
If you don’t take an MVM supplement or your use of them is sporadic and strategic, remember that various forms of cooking have a significant effect on the nutritive value of veggies, fruits, and meats.
For example, if you cook (and drain the boiling water from) a stalk of broccoli, with the assumption that you will be ingesting fantastic amounts of vitamin C and B12, keep in mind that the boiling itself may reduce the vitamin content by 75 percent and 50 percent, respectively.6
Note
A study showed varying effects of boiling on veggies such as broccoli and asparagus.7 For asparagus, boiling actually raised its “[free] radical scavenging activity,” or RSA (a measure of antioxidant activity), by 10 percent, and 15 percent of the original vitamin C content of the veggie was left in the cooking water. Broccoli retained only 83 percent of its RSA after boiling, and the cooking water had a high antioxidant value as well.
There are many solutions to this conundrum. If you’re cooking a stew, then make sure you consume the broth with the stew contents, because this liquid will likely contain some of the nutrients.
If you boil veggies on occasion, you can be hardcore like me: take the leftover boiling water and use it as a base or an ingredient for a smoothie. The study referenced by the last note pointed out that a stalk of boiled broccoli, for instance, leaves about 28 mg of its vitamin C in the cooking water (the water alone containing about a fifth of a good day’s worth of C for the average person). For sure, the water tastes a little weird at first, but be creative, as in the upcoming sidebar.
You can also impress your friends and appall your guests by simply guzzling the leftover water out of the pan.
As we saw in Chapter 2, there are many handy tools for helping determine the nutritional content, or lack thereof, of your diet. We’ll take another look at some of these, and introduce a few new ones, in “Getting Micronutrient Information Online: Web Tools,” at the end of this chapter. The FitDay on Vending-Machine Fare section gives the lowdown on some of the “food-like substances” some of us geeks like to eat.
If you’re like me, you pretty much slept, or teased Gilda McGillicuddy in the seat next to you, when the elementary school nurse bopped in for a lecture on “The Importance of Vitamins.” The following sections contain a wealth of knowledge about vitamins and minerals, and I’ve designed it to be a digestible and concise package. You can even skip over it to the online tools section at the chapter’s end and just return to this section for later reference.
The Linus Pauling Institute’s Micronutrient Information Center at Oregon State University is one of the best places around for finding out more detailed biochemical information about these substances: http://lpi.oregonstate.edu/infocenter/. Whenever possible, each nutrient has a reference back to the LPI pages.
Vitamins are organic molecules (the ones containing carbon atoms) that are cofactors or helper molecules for enzymes that play vital roles in the body. Back in the early part of the last century, the term “vitamin” was formed from “vital amines,” when it was thought that all vitamins were amine molecules.
Vitamins aren’t used for energy themselves, but they are crucial for many of the internal chemical reactions by which our body’s machinery can utilize protein, carbs, and fat for fuel.
Food scientists don’t consider a nutrient a vitamin unless it’s essential for our metabolism or other vital systems, and must be obtained via the diet. Monkeys, apes, humans, and some birds, for example, have lost the ability to synthesize vitamin C. We can biosynthesize vitamin D from exposure to ultraviolet (UV) light from the sun, however, and some bacteria in our guts can synthesize vitamin K, a fat-soluble vitamin.
Enzymes are biochemicals (usually proteins) that catalyze or initiate chemical reactions but are not used up by those reactions. Enzymes commonly end with the suffix “ase,” as in lactase, the enzyme that allows people to digest milk sugar or lactose, or the enzyme in saliva that disassembles starch into smaller sugars, amylase.
We don’t use up vitamins for energy, as we do carbohydrates or protein in food, but they take part in numerous essential chemical reactions, or simply are hormones themselves, like the active form of vitamin D.
Even though vitamin D might get all the splashy headlines these days, the eight B-complex vitamins and vitamins A, C, E, and K also play crucial roles in the basic physiological processes that keep us alive.
A subset of vitamins can be stored in body fat and are thus described as “fat-soluble.” This characteristic has two main ramifications. First, to properly absorb these vitamins in supplement form, it helps to consume them with a little dietary fat (e.g., a blob of Greek-style yogurt). Furthermore, eating healthy fats, like a pastured egg, an avocado, or coconut milk, will help you derive more fat-soluble vitamins, because the fats you are digesting contain the nutrients.
Second, since fat-soluble vitamins can be stored, you can potentially overload your body with fat-soluble vitamin supplements. Although it’s difficult to do, you could, for example, take in too much vitamin A in cod liver oil and potentially accumulate toxic levels of this vitamin.
Note
An upcoming section is devoted to vitamin-A toxicity, or hypervitaminosis A. For an article that goes into more scientific detail, see http://lpi.oregonstate.edu/infocenter/vitamins/vitaminA/.
This is the reason why you shouldn’t start taking mega doses of vitamin A (or any supplement, for that matter) without reading the supplement labels and checking the RDA for adults and kids first (see the sidebar earlier in this chapter on reading the Supplement Facts label).
The fat-soluble vitamins are vitamins A, D, E, and K.
Note
I made up my own mnemonic device for remembering them: “a deck of cards,” ADEK. It’s a start, right?
This vitamin is available in the diet in two forms:
Retinol, or preformed vitamin A (“true” vitamin A) from animal sources like eggs, pastured butter, fish, meats, and cod liver oil.
Pro-vitamin A carotenoid, the vegetable- and fruit-based beta-carotene (found in orange and other brightly colored foods like carrots, cantaloupes, peaches, sweet potatoes, and leafy veggies), which the body can convert into retinol, albeit at a low conversion ratio.8
There is an international conversion factor for foods and supplements called the retinol activity equivalents (RAEs), described in the upcoming “Retinol Activity Equivalents for Vitamin A” sidebar. For example, 12 units of beta-carotene are about the equivalent of 1 unit of vitamin A or retinol.9
Beta-carotene is also an effective antioxidant.
You could theoretically (given the cooking method and your individual ability to incorporate food; i.e., no potential digestive problems, age, etc.) acquire all the vitamin A you need for a day from a medium-sized carrot, a baked sweet potato, and a salad ingredient of spinach. In fact, that would probably give you more than you need (unless you’re an athlete putting in mega miles).
The body converts retinol from these various forms of vitamin A into retinoic acid, which is the molecule responsible for vitamin A’s biological effects.
For example, retinoic acid affects gene transcription, and thereby affects how certain bodily proteins are synthesized (some tissues have retinoic acid receptors, or RARs).10
Vitamin A is essential for the health of your retinas, particularly for night vision. If you bump up your vitamin–A containing veggie intake after a period of deficiency, you might notice the night-vision difference right away. As you’re driving at night, can you read the small print on those luminescent street signs?
Vitamin A has a crucial anti-infective role in the immune system. Retinol is required in the body for the normal functioning of epithelial cells, the “first line of defense” that line the airways and digestive tract, for instance. The body needs vitamin A to develop white blood cells such as lymphocytes, which are central to our immune system.11
“Vitamin A appears to facilitate the mobilization of iron from storage sites [in the body] to the developing red blood cell for incorporation into hemoglobin, the oxygen carrier in red blood cells,” according to the online Linus Pauling Institute (LPI) article at http://lpi.oregonstate.edu/infocenter/vitamins/vitaminA/index.html#function.
Since vitamin A is a fat-soluble vitamin, it is possible to take too much preformed vitamin A (you do not get vitamin A toxicity, or hypervitaminosis A, from eating a lot of carotenoids, as found in carrots, bell peppers, sweet potatoes, and mangos, for instance).
Although fairly rare, hypervitaminosis A has serious symptoms, such as liver abnormalities, reduced bone density, and cerebral edema (what occurs with the onset of the severe form of high-altitude sickness). Most people fully recover by simply stopping the overdosing of A.
Check the tolerable upper limit (TUL) for vitamin A before you start imbibing a lot of preformed vitamin A in the form of supplements or cod liver oil, for example.13
Note
Vitamin A amounts are specified in IUs. To convert IUs to micrograms: 1 IU of A equals 0.3 micrograms.
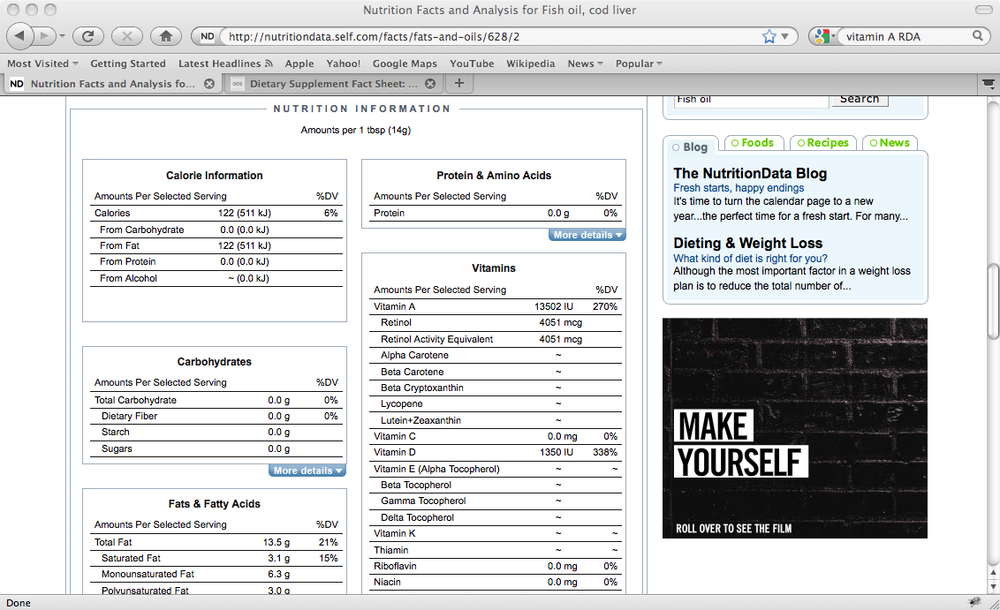
I did a search on cod liver oil at www.nutritiondata.com. Figure 4-2 shows what I found. Look at that retinol amount for just one tablespoon: 4,051 micrograms. The TULs specify that adults shouldn’t take more than 10,000 IU or 3,000 mcg of retinol per day, and kids aged four to eight should take no more than 3,000 IU or 900 mcg.14
Again, it is quite easy to get enough vitamin A by eating whole foods such as vegetables that contain carotenoids, salmon (an RAE of 229 mcg), and two scrambled eggs (an RAE exceeding 600 mcg).
If ever a vitamin could be deemed “sexy,” it would be vitamin D.
The hype surrounding vitamin D seems to be spreading: a very tanned checkout girl, who looked like she’d recently broken Owen Wilson’s and Matthew McConaughey’s hearts (at the same time), recently told me she’d spent the weekend “getting her vitamin D” (and she probably did get her D that way).
Everywhere you look, another “media story based on a study” touts the vitamin’s multifarious benefits.
The hype seems to have at least a partial basis in fact.
Photosynthesis has generated vitamin D in life forms on earth for millions of years, and it is a remarkable biosynthetic mechanism by which we can create a vital chemical for our bodies from sunlight.
We’re like plants, basking in the sun for reasons much more important than an excuse to wear Ray-Bans.
The human genome has hundreds of sites known as vitamin D receptors (VDRs), indicating that the active form of vitamin D can bind with these sites and affect gene expression (meaning some “health-positive” genes can be turned on, and/or genes that have negative effects can be switched off).15
Along with sunblock, which will screen out the ultraviolet (UV) rays that help produce vitamin D, modern life—specifically, Facebook, Twitter, Netflix, cubicle life, and every other excuse to sit in a glorified box in front of a screen—has driven us indoors, where we were never really designed to spend a lot of time in the first place.
Back in my own software engineering days, I tried to walk in the sun as much as possible during the workday. I walked half an hour or more every morning from the train along Cambridge, MA’s sunny sidewalks (yeah, the sun comes out in New England, sometimes). I went outside several times a day to find splotches of sun in Kendall Square. Right now I’m headed off to sit on a rock in the sun and swim in a Vermont waterway called the Mad River. Of course, I take some D supplements too. I do spend the winter in New England, a region and time of year not usually known for sunshine.
Your vitamin D status is a relevant marker of health. A Massachusetts General Hospital study found that among 290 patients entering the hospital with a variety of ailments, about 57 percent of them were vitamin D–deficient, with blood levels of 15 ng/ml (nanograms per milliliter) or less.16
A September 2009 study of more than 3,000 older folks in the U.S. found that “compared [with] those [who had] optimal vitamin D status, those with low vitamin D levels were three times more likely to die from heart disease and 2.5 times more likely to die from any cause.”17
Here’s how we naturally produce our own vitamin D. The skin generates cholecalciferol, the inactive form of vitamin D, when cholesterol molecules in epidermal cells are exposed to ultraviolet radiation.18
The liver converts this biochemical to calcidiol, or 25-hydroxyvitamin D, abbreviated 25(OH)D—a prehormone and the form of vitamin D that blood tests detect (see the Testing for D section). A prehormone is a substance that other tissues in the body convert into an active hormone, a signaling chemical that binds with receptors and launches chemical reactions in the body.
It’s good to know all this stuff because you’re probably going to be testing for vitamin D, and the doctors will be casually tossing around terms like “25(OH)D.” Besides, you can also impress tanned checkout girls (or guys) with your advanced vitamin-D know-how!
An enzyme in the kidneys called 25(OH)D-1α-hydroxylase further modifies this chemical calcidiol to calcitriol, or 1,25-dihydroxyvitamin D. This is a secosteroid hormone that is responsible for most of vitamin D’s physiological effects. A secosteroid hormone is similar to a steroid hormone like testosterone and estrogen, but has a slightly different molecular structure.
This hormone binds with hundreds of sites throughout the body that have vitamin D receptors, and thereby affects how many of our genes are expressed.
Vitamin D is an essential molecule for bone health, but it has also been associated with promoting insulin sensitivity (where your cells are able to admit glucose and amino acids in response to the presence of insulin in the bloodstream), preventing the cell proliferation associated with certain cancers such as those of the prostate, breast, and colon, as well as helping prevent high blood pressure.19
Along with exposure to the sun, you can also build up your vitamin D with food and supplements.
Some foods are fortified with vitamin D3 (like milk, about 115 to 124 IU per 8 ounces20), or contain moderate vitamin D3 levels without fortification (grass-fed or free range eggs and salmon). A can of sardines has about 250 IU of vitamin D3, but that’s not enough for a day.
The sun might still be the best way to get vitamin D, for the same reason we drink water through our mouths instead of running off to inject it intravenously—because that’s the way we’re designed. It’s also impossible to develop vitamin D toxicity from the sun, unless you’re also taking too high a dose in supplemental form. My guess is that surfers and lifeguards who aren’t covered by a wetsuit and sunblock all the time have pretty healthy D levels.
Note
A recent study of some people in East Africa who live pastoral or hunter-gatherer lifestyles, the Maasai and the Hadzabe, noted that their mean 25(OH)D levels fell into the mid to high-40s range. The Maasai’s mean levels were “48 ng/ml (119 nmol/L) and ranged from 23 to 67 ng/ml,” and the Hadzabe’s were “44 ng/ml and ranged from 28 to 68 ng/ml.” A “deficient” level, according to U.S. standards, is beneath 32 ng/ml (see http://blog.vitamindcouncil.org/2012/01/25/new-study-vitamin-d-levels-of-the-maasai-and-hadzabe-of-africa/).
But what about those of us who live in the northern latitude—not near the equator, in Australia, or in the U.S. sunbelt—or have a darker skin color, which makes it more difficult compared with lighter-skinned people to make D from the sun (especially in northern regions)?
Note
Obesity also makes photosynthesized vitamin D less bioavailable. See http://hjira.com/acjn/72-3-690.full.pdf.
Vitamin D3 supplements are cheap (about $30 per year for a daily 2,000 IU dose, the last time I looked) and readily available. The National Institutes of Health (NIH) has recommended that adults, kids, teens, and pregnant women take 600 IU per day, the minimum amount necessary for bone health. As for blood levels, “levels ≥50 nmol/L (≥20 ng/ml) are sufficient for most people,” according to an NIH fact sheet.21
Note
In terms of vitamin D, 40 IU equals 1 microgram (mcg). So if you take a 4,000 IU dose daily, you’re getting about 100 mcg.
However, the Vitamin D Council, an advocacy group, recommends that both adults and kids should attain a D serum level of about 50 ng/ml (125 nmol/l).
There is obviously some disagreement between the recommended levels of the federal government and the Council, which suggests that the public-health recommendations move too slowly to track the latest D research findings. In other words, the active form of vitamin D affects much more, physiologically, than calcium and bone health.
You could take the conservative approach and consider the U.S. government’s recommended dose, then test to determine if the supplement’s effects are adequate. Also see this page for the Vitamin D Council’s recommended amounts and its rationale: www.vitamindcouncil.org/about-vitamin-d/how-to-get-your-vitamin-d/vitamin-d-supplementation.
If you’re vitamin D–deficient, there seems to be some evidence that remedying that condition will aid an athlete’s or a weekend warrior’s sports performance. See the “Better D Status Boosts Sports Performance” sidebar.
To reach the higher levels in your blood tests, in almost all instances, you would have to take more supplemental D3 than the NIH’s recommended 600 IU per day, although how the body responds to vitamin D3 supplements varies from one person to the next. Some adults may attain healthy levels with 600 to 2000 IU per day; for others, it may take 4,000 IU or more per day.
Fat-soluble vitamins can be stored in human adipose tissue, so toxicity is possible when thoughtlessly supplementing with vitamins A and D, for instance, especially for kids. Their low body weights make them more vulnerable to toxicity when their dosages are recklessly scaled upward. An adult dose of 5,000 IU per day will not have the same effect on a kid who weighs 50 pounds.
The federal government puts the TUL for D3 at 4,000 IU per day for males and females of age 9 and above, “while symptoms of toxicity are unlikely at daily intakes below 10,000 IU/day.”22
Other D3 researchers have noted that the TUL could be much higher than that, since about 30 minutes of full-body, high-noon sun exposure will generate up to 20,000 IU naturally.
“Excessive sun exposure does not result in vitamin D toxicity, because the sustained heat on the skin is thought to photodegrade previtamin D3 and vitamin D3 as it is formed,” according to a National Institutes of Health Dietary Fact sheet on vitamin D. For more information, see http://ods.od.nih.gov/factsheets/vitamind/#h8.
Testing your D3 levels involves asking your doctor to have it included in a blood workup during a typical routine checkup or using one of several private testing services.
The result will be in the form of a number representing your blood level of 25-hydroxyvitamin D. In the U.S., this will most likely represent a 25-hydroxyvitamin D (sometimes shortened to “25 (OH) D”) level in nanograms per milliliter (ng/ml), a figure like “48 ng.”
Other countries, like the United Kingdom, may provide this number in nanomoles per liter (nmol/L), resulting in a number that is about 2.5 times higher (48 ng is 120 nmol/L).
According to the NIH, levels greater than 20 ng/ml are “generally considered adequate for bone and overall health in healthy individuals,”23 but other researchers or advocates, such as the Vitamin D Council, advocate a higher number—50 ng/ml or more.
Science Daily reported on a February 2011 study that found much higher daily doses of vitamin D were required to protect most adults from cancer. “We found that daily intakes of vitamin D by adults in the range of 4000–8000 IU are needed to maintain blood levels of vitamin D metabolites in the range needed to reduce by about half the risk of several diseases—breast cancer, colon cancer, multiple sclerosis, and type 1 diabetes,” according to a doctor at the UC San Diego Moores Cancer Center.24
Vitamin E is one of the body’s primary antioxidants. Since it’s stored in body fat, vitamin E helps prevent the destruction by free radicals of the fats in cell membranes. Fats are a major component of cell membranes, so vitamin E has a key role in cell biology. Vitamin E also helps combat the oxidation by free radicals (the bad guys, when they’re not being used to destroy invading germs) of low-density lipoproteins or LDLs.
LDLs are protein-fat-cholesterol complexes that travel through the bloodstream.
Vitamin C helps regenerate the antioxidant capacity of vitamin E—an example of two vitamins working synergistically and why you should aim to keep up to speed on all vitamins.
The liver secretes a form of vitamin E called alpha-tocopherol.25
Naturally sourced vitamin E is called d-alpha-tocopherol; the synthetically produced form is dl-alpha-tocopherol.26
The RDA for adults from adolescence on is 15 mg. One ounce of almonds, about 23 nuts, gives you 7.4 mg, which is almost half of the vitamin an adult needs to reach the RDA. Avocados (providing 4.5 mg, about a third of the RDA), olive oil, Swiss chard, spinach (cooked and raw), asparagus, and sunflower seeds are also very good sources of vitamin E.
Some studies have cast doubt on the efficacy of supplementing with vitamin E, as well as C for that matter, according to the National Institutes of Health in the U.S.27 On the other hand, supplementing up to the RDA for these vitamins in most cases can’t hurt. For a vitamin C–related supplement discussion, see the Vitamin C: Helps Keep Your Tissues and Fat-Burning Capabilities Intact sidebar.
Vitamin K, another fat-soluble vitamin, plays an important role in blood clotting (the “K” comes from the German word “koagulation”), bone health, and preventing or reducing the calcification of arteries.
There are two naturally occurring forms, broadly referred to as K1 (phylloquinone) and K2 (menaquinone). The easiest way to think of vitamin K is that it puts calcium where it belongs (the bones) and removes it from where it doesn’t belong (the arteries).
Plants manufacture K1, which is the vitamin K that newborn infants are given (I found it jarring—as the “husband witness,” milling around somewhat ineffectually—when immediately upon both of my children’s births, they were jabbed in the leg with a vitamin K1 shot, even before being wrapped in a blanket). The usual healthy suspects—parsley, spinach, leafy green lettuce, kale, broccoli, and olive oil—are good sources of vitamin K1.
Some bacteria in the large intestine generate K2, one of the few instances where a vitamin can be synthesized in the body (see below for the food sources of this nutrient).
Note
Why should you even think about foods and supplements containing K2, if the gut flora can synthesize it? Because antibiotics can kill the bacteria in your gut that produce it, and it’s a fairly important and underestimated vitamin that calls for insurance measures to make sure you’re getting enough.
The bacteria make a range of K2 designated as MK-n (MK-4 in meats or supplements; MK-8 or 9 in cheese), where “n” stands for a 5-carbon unit on the side of the molecule, according to the Linus Pauling Institute’s page on K2: http://lpi.oregonstate.edu/infocenter/vitamins/vitaminK/.
For example, menaquinone-4 (MK-4) means the molecule has four 5-carbon units.
Grass-fed cheese appears to be a good source of K2, according to Mark Sisson’s Mark’s Daily Apple page: www.marksdailyapple.com/cheese-unhealthy/.
Cheddar cheese, Swiss cheese, eggs, and chicken contain MK-4 in higher amounts than other foods.28
These comments on vitamin K2 contained in cheese and Natto (a fermented soy food popular in Japan that is a very good source of minerals and protein), from a 2004 Dutch study published in the The Journal of Nutrition, are eye-openers:
Cheese has not been established as a dietary risk factor for cardiovascular disease in epidemiological studies, despite its high levels of saturated fat and salt. We hypothesize that menaquinones in cheese (MK-8 and MK-9) could exert a beneficial effect in the cardiovascular system and that the high cheese consumption in France and the Mediterranean countries may possibly account for lower prevalences of [heart disease].{...]
In healthy Japanese subjects who consumed fermented soybean (Natto) high in menaquinone (especially MK-7), serum concentrations of MK-7 and carboxylated osteocalcin were significantly increased.29
K2 activates a protein called osteocalcin that builds or remodels bones by binding calcium to a mineral matrix. In fact, K2 works together with vitamin D and calcium to keep your skeleton healthy and strong. The active form of vitamin D, calcitriol, plays a role in the synthesis of osteocalcin.
Another vitamin K–dependent protein called matrix Gla protein (MGP) helps prevent the calcification or hardening of soft tissue and cartilage. Runners and cyclists, keep that one in mind as you consider vitamin K2 supplementation.
The water-soluble vitamins do not have to be eaten with fat to be absorbed, and it’s harder to overdose on these vitamins, as the body can flush them out via the urine. This doesn’t make these substances—the eight B-complex vitamins and vitamin C—any more innocuous or less important than the fat-soluble ones, though. Some of the most infamous nutrient-related diseases are caused by deficiencies in C (scurvy), thiamine (beriberi), and niacin (pellagra).
This group of eight vitamins—B1 (thiamine), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid), B6, B7 (Biotin), B9 (folic acid), and B12—has a wide variety of vital roles in the body. The MVM supplements will refer to the whole group of them as a B-complex vitamin.
Your first question might be: what about all those missing Bs (B4, B8, B10, etc.)? The short answer is that scientists decided that they weren’t “vitamins” anymore, for reasons such as the body’s ability to synthesize them.
Thiamine (B1) was one of the first vitamins ever discovered, in the late nineteenth century. “The story of thiamine is the story of beriberi, the disease caused by thiamine deficiency.”30
In the early 1880s, for example, a Japanese naval physician named Kanehiro Takkaki found that adding meat, fish, and vegetables to the white-rice seaman’s staple helped to cure a disease that had cut a swath through sailors, many of whom had languished on a low-level diet of polished white rice.
Note
When you remove the brown skin on rice, usually accomplished by milling machines, to make “polished white rice,” even the tiny amounts of thiamine present in brown rice are lost. Beriberi, the horrible disease that has been common in populations that depend on rice in their diets, is broken down into “dry,” “wet,” and “cerebral” beriberi (see http://lpioregonstate.edu/infocenter/vitamins/thiamin/).
Thiamine plays a number of crucial roles as a coenzyme (an essential assistant for an enzyme) in basic metabolic processes.31
Transketolase, for example, is a key enzyme for synthesizing DNA and RNA, among other biochemicals. Its presence in diminishing amounts in red blood cells is taken for a possible sign of thiamine deficiency.
The RDA of thiamine is only 1.2 mg for an adult male and 1.1 mg for females. Three scrambled eggs provide just 0.1 mg, the same amount you get from a cup of plain yogurt, about 4 ounces of cooked brown rice, or one slice of beef liver. Thiamine tends to be in lots of foods in tiny amounts.
B2 (riboflavin) is involved in the metabolism of food (carbs, protein, and fats), as well as in the formation of other B vitamins such as niacin into their corresponding coenzymes.
B2 is an integral part of a coenzyme that assists glutathione, for example, one of the body’s major built-in antioxidants.32
Similar to B1, the riboflavin RDA is 1.3 mg for adult males and 1.1 mg for females 19 and older. An apple (0.1 mg), a small Atlantic salmon filet (0.7 mg), and a hard-boiled egg (0.3 mg) get you most of the way there, according to NutritionData.
Niacin (B3) is also known as nicotinic acid, but it has no relation to the nicotine in cigarettes.33
Severe deficiency in B3 vitamins can cause pellagra, a disease whose name may be derived from the Italian words for “rough skin.”
Note
Pellagra is considered the disease of the four Ds: dermatitis, diarrhea, dementia, and death. As explained in Frances R. Frankenburg’s book Vitamin Discoveries and Disasters, once the Europeans imported maize, or corn, from North America, pellagra began to spread in Europe. Maize is a cheap source of calories, but not of good nutrition; the niacin (B3) is bound and not absorbed unless the corn is soaked in limewater or another alkaline solution—a process called nixtamalization—as is done to make Mexican tortillas. The preColumbian and preHispanic populations of the Americas did not have the same problems, because they knew how to mix corn with other foods.
The liver can also synthesize B3 from the amino acid tryptophan (an amino acid is a building block for proteins), but it takes a lot of tryptophan (60 mg) to make 1 mg of B3. As an amino acid, tryptophan is a component of good protein sources like turkey, salmon, eggs, and whey protein. For example, half a filet of salmon will give you about 450 mg of tryptophan (along with many other amino acids).
The RDA for niacin is 16 mg per day for an adult male, and 14 mg for a female. That tasty filet of salmon will give you about 14 mg of niacin alone: other good sources include a 6-ounce serving of chicken breast (almost 20 mg), turkey (a little less than chicken), half a can of tuna (about 5 mg), and an avocado (about 3 mg).
Vitamin B5, or pantothenic acid, is essential for all forms of life, due to its conversion to coenzyme A (CoA).34 CoA is a cog in a central metabolic pathway of biology called the Krebs or citric acid cycle, by which cells generate energy from food sources.
The adequate intake (AI) for pantothenic acid, since it doesn’t have an RDA, is 5 mg per day for adults. You can get vitamin B5 pretty easily from foods: a small piece of wild Atlantic salmon has 3 mg, half a chicken breast has about 1 mg, and a California avocado has 2 mg.
Vitamin B6 is a coenzyme for glycogen phosphorylase, an enzyme involved in the cleaving of glucose from glycogen (the way the body stores starch in the muscles).
Glycogen is a long chain of glucose molecules. When your muscles need energy (you’re standing up now, right?), the muscle cells look to acquire it from glycogen, which is like their own food pantry.
Note
The muscles also have their own stored fats, from which they derive a substantial amount of their fuel. Interestingly, the fats inside muscles store more energy in calories than the total amount of glycogen that your body stores.
The chain of glucose molecules that make up glycogen has to be broken up into the separate pieces of glucose so that cells can use the latter for energy (see Chapter 3).
Coenzymes are like an enzyme’s essential assistant; they bind with the enzyme and are a part of the chemical reactions that enzymes initiate.
B6 is also a coenzyme in the production of glucose or fuel from protein, a pivotal metabolic process called gluconeogenesis. Reactions that are dependent on B6 are also involved in the nervous system, such as generating serotonin from the amino acid tryptophan, and synthesizing the neurotransmitters dopamine and norepinephrine.35
Vitamin B7 (biotin) is also an enzyme cofactor.36 Remember that scene from Rocky when Rocky Balboa chugged the raw eggs before heading off on another Philadelphia jaunt? Well, think twice. Raw egg whites contain a chemical called avidin that binds to biotin, prevents its absorption, and can lead to biotin deficiency.37
The AI for biotin or B7 is 30 mcg per day for an adult.
Folates are the form of vitamin B9 found in food, while folic acid is the synthetic form found in supplements and fortified foods.
The U.S. government has required breads, cereals, flours, corn meals, pastas, rice, and other grain products to be fortified with folic acid since 1996, because people eat these foods in large amounts, and the grains are poor natural B9 sources. The RDAs for B9 are based on a term called dietary folate equivalent (DFE).
According to the NIH fact sheet for folate, “DFE accounts for the easier absorption of folate in supplements and fortified foods compared with folic acid found naturally in foods, which is absorbed only about half as well. One DFE = 1 microgram food folate, which = 0.6 microgram folic acid from supplements and fortified foods.”38 So, the DFEs are 600 mcg per day for pregnant women, 500 mcg for lactating women, and 400 mcg per day for adult men and other women.
Broccoli, asparagus, and spinach are good sources of folates, along with the fortified breads and other foods. For example, only eight spears of boiled asparagus will give you about 180 mcg of B9, and a pretty big spinach salad or two hard-boiled eggs provides about the same. Two tablespoons of saltless peanut butter only give you about 24 mcg of B9.
Note
Which is better for B vitamins, a grass-fed or non-grass-fed beef steak? A quick search on NutritionData shows that a similar gram-weight of grass-fed steak has more niacin, folates, B6, and pantothenic acid, sometimes by a magnitude of two or three, than the other steak (http://nutritiondata.self.com/facts/beef-products/10525/2). The exception is B12: both are good B12 sources, and the conventional steak provides almost all you need.
Vitamin B12 is a cofactor for several enzymes. These include molecules that help synthesize DNA and build hemoglobin, which carries oxygen in the blood throughout the body. This is why B12 deficiencies can lead to anemia, an inadequate number of red blood cells.
Vitamin B12 is mostly found in animal products like fish (including good sources like shellfish), beef, turkey, and chicken, as well as dairy products like eggs, milk, and cheese. Plant foods do not contain B12, so vegetarians have to obtain it by eating dairy products or with supplements. Two pastured eggs, hard-boiled, and a cup of whole milk will get you all the way there.
The RDAs for B12 are 2.4 mcg for adults, and a bit more for pregnant or lactating moms.39
Also called ascorbic acid, this vitamin from fresh fruits and veggies is pivotal for many reasons, which is why you were harangued so much as a child to eat your apples and drink your OJ. For one, it is essential for synthesizing the protein-containing structural component of ligaments, bones, tendons, and blood vessels called collagen (see the accompanying sidebar on vitamin C).
The body also uses vitamin C “as a cofactor for catecholamine biosynthesis, in particular the conversion of dopamine to [the neurotransmitter] norepinephrine,” according to an article in the American Journal of Clinical Nutrition.40
Vitamin C is a powerful aqueous-based antioxidant. It helps mop up the reactive oxygen species in the watery parts of cells. It also helps recharge vitamin E after that vitamin has neutralized oxidative stress in the fatty parts of cells, such as their membranes.
Vitamin C deficiency is infamous for causing scurvy, a potentially fatal disease that beset British sailors in the 17th and 18th centuries, and it still rears its ugly head in the modern world.
Note
During the 1941 siege of Leningrad in World War II, an epidemic of scurvy swept through Russian civilians, who’d been given only bread rations. Pine needles boiled in water (pine needle tea) helped stave it off, as pine needles are rich in vitamin C.41
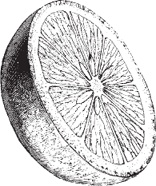
The RDA for vitamin C is 90 mg per day for male adults and 75 mg for females, but supplements as well as fruits and veggies typically provide the body with far more than that amount. For children aged four and older, the RDA rises incrementally from 25 mg to about 75 mg per day. Apples provide about 10 mg each, oranges about 68 mg, and a cup of lemon sections more than 100 mg, according to NutritionData.
I’ve taken to eating lemons raw or adding raw sections to smoothies, because they are very high in vitamin C and low in fructose (see Chapter 3 for a note on fructose) compared to a typical sweet apple.
A medium-sized apple contains almost 11 grams of fructose (and 8.4 mg of vitamin C), compared with a medium lemon (less than 1.5 grams of fructose and about 31 mg of vitamin C).
If you munched a clump of raw broccoli in a salad (however torturous that may sound to some), you’d derive about 66 mg of C, according to NutritionData.
Essential minerals are inorganic substances from the earth that must be provided by the diet. They include calcium, phosphorus (phosphates), magnesium, sulfur, sodium chloride (salt), and potassium, as well as the “trace” minerals of which fewer milligrams are required per day. These include iron, zinc, copper, manganese, iodine, selenium, fluoride, molybdenum, and chromium.
You can get minerals from your MVM supplement, as well as from both food and beverages. For example, drinking water from streams or aquifers (e.g., a commercial mineral water) could provide some of the minerals needed by your body.
The adequacy of the minerals you derive from food is directly related to the mineral richness of the soil the food was grown in. This is why we included a chapter in this book on the filial loyalty you should display toward all your local farms. Some processed foods are also fortified with minerals, such as bread fortified with iron or orange juice with calcium.
A whole-foods diet dominated by local vegetables and fruits that are in season or frozen at their peak of freshness, as well as healthy meats and cheeses, should provide many of the minerals you require in adequate amounts.
Minerals, like vitamins, play numerous roles in the body that belie the quantities consumed. Many minerals are constituents of life-giving molecules, like the iron in hemoglobin (red blood cells), which transports oxygen throughout the body; the phosphorus that is a part of adenosine triphosphate (ATP), which is the form of energy that our cells use; and the iodine that the thyroid gland uses to make thyroid hormone.
These are the major minerals that are required in the body in quantities of about 100 milligrams or more per day: calcium, phosphorus (phosphates), magnesium, sulfur, sodium chloride (salt), and potassium.
About four percent of the body’s weight is made up of minerals, with three quarters of that amount in calcium and phosphorus.42 The vast majority of calcium resides in the bones and teeth, but calcium also plays a critical role in the extracellular fluid, among other places. Along with other biochemicals, calcium affects the permeability of cell membranes during the exchange of substances like oxygen, nutrients, and metabolic waste products.
Calcium’s function is so important in the extracellular fluid that if you don’t have enough calcium in your bodily fluids, the body will free up calcium from your bones, or “demineralize” them. This is why it is important to get enough calcium in your diet.
Once the body senses a calcium deficit, it releases parathyroid hormone, which signals the kidneys to produce more of the active form of vitamin D. The active form of vitamin D, calcitriol, stimulates the absorption of calcium from any food in the small intestine, as well as the demineralization of bone if the latter source is inadequate. You can see how vitamin D and calcium work together.
Adults and adolescents should get about 1,000 to 1,300 mg per day of calcium (the RDA for pregnant and lactating moms over 18 years of age is 1,000 mg). Good sources of calcium are dairy (milk, cheese, and yogurt), as well as green vegetables like spinach and Swiss chard.
However, vegetables such as spinach, while containing a lot of calcium, also contain large amounts of oxalic acid, which can bind with and prevent the absorption of calcium. (See the upcoming sidebar Going Against the Grains: Plants Contain “Antinutrients”.) Cooking breaks down the oxalates, which generally do not prevent the absorption of calcium from other foods you are eating at the same time, like cheese or yogurt.
Magnesium is required by the chemical reactions that make ATP, our primary energy currency, in the mitochondria of cells, according to the Linus Pauling Institute (http://lpi.oregonstate.edu/infocenter/minerals/magnesium/). The adult human body includes about 25 grams of magnesium, mostly in bones.
The synthesis of glutathione, a natural antioxidant in the body, requires magnesium. Magnesium also plays a structural role in bone, cell membranes, and chromosomes, according to LPI. And it goes on and on. Obviously, you have to get enough magnesium in your diet.
The magnesium RDA for males (i.e., the minimum amount you should get, give, or take) is 420 mg per day, and for females it’s 320 mg per day. According to NutritionData, here are some examples of common magnesium sources:
2 cups coffee: 14.2 mg
2 squares baking chocolate: 190 mg
8 ounces grass-fed ground beef: 38 mg
8 ounces whole milk: 24.4 mg
1 cup spinach: 23.7 mg
1 cup Swiss chard: 150 mg
5–6 ounce filet of haddock: 75 mg
2 ounces cheddar: 15.6
2 Florida oranges: 28.2 mg
Cacao, a good source of which is high-cacao chocolate, is a rich source of magnesium. The surprising sources to me were chard and haddock, providing about half of all you would need in a day. Oranges are also a surprisingly good small source.
This exercise is also a good indication that you can derive your nutrition from commonly eaten whole foods, which obviously contain far more vitamins, minerals, and phytochemicals than just magnesium.
Phosphorus is another major nutrient for your bones; about 85 percent of this mineral in the body is found there. A phosphates-and fatty acid–containing structure called phospholipids is a principal component of all body cell membranes. Last but not least, the primary energy currency of the body, a molecule called adenosine triphosphate (ATP), also contains this mineral, as do DNA and RNA, which are long chains of phosphate-containing molecules.43
Phosphorus has the same interaction with vitamin D as calcium when the body detects blood levels falling beneath a certain level. Parathyroid hormone sends the message to increase the generation of the active form of vitamin D in the kidneys, which in turn increases the amount of phosphates (and calcium) absorbed from the intestines.
People generally get enough phosphorus in their diets, which unfortunately includes the burden of food additives that contain phosphates. The RDA for phosphorus is about 700 mg per day for adults and 1,250 mg for children between 9 and 18 years old. Good natural sources (nonfood additives) of phosphorus are milk, yogurt, cheese, eggs, meat, and fish.44 A vegan, however, eschewing both meat and dairy products, may have trouble getting enough phosphorus in her diet.
People should generally keep their potassium to sodium (or salt) intake ratio at about 4 to 1. In other words, you should get about four times as many milligrams of potassium as salt. Researchers have pointed out that we’re ultimately designed to have a high potassium-to-sodium ratio in our diet, and recent studies have underlined this point.
“Americans who eat a diet high in sodium and low in potassium have a 50 percent increased risk of death from any cause, and about twice the risk of death from heart attacks,” according to a study published in July 2011 in the Archives of Internal Medicine.45
Here’s a good list of useful potassium food sources with great potassium-to-sodium ratios:
Medium-sized kiwi: 237:2
5–6 ounces salmon: 967:86
One large stalk cooked broccoli: 820:115
4 ounces grass-fed ground bison: 353:76
Medium-sized lemon: 80:1
One cup raw spinach: 167:24
California avocado: 689 mg:11
One cup raspberries: 186:1
One cup cherry tomatoes: 147:3
One cup blueberries: 114:1
One medium-sized banana: 422 mg:1
In other words, a small piece of wild salmon gives you about 1,000 mg (or 1 gram) of potassium, and confers a potassium-to-sodium ratio of more than 10:1.
So what does potassium do? The concentration of potassium inside a cell is about 10 times the concentration outside, and for sodium the ratio is reversed (other sources have different estimates for this concentration).46 This creates a conveyor belt or “ion pump” across cellular membranes, a gradient that enables the basic machinery throughout the body: nerve cell signals, muscle contractions, the heart’s cardiac output, as well as the transport of glucose fuel, for example, from outside to inside the cell.
An endurance athlete can run dangerously low on potassium, and this is partly what causes any muscle spasms and cramps.
Adults require about 4,700 mg per day of potassium (children less than 14 years old need 3,000–4,500 mg per day). It is relatively easy to derive your necessary potassium from a whole foods diet, as the above list shows.
Along with potassium, salt makes up the sodium-potassium pump that is a basic part of cellular mechanisms (e.g., nerve transmission and muscle contraction).
You should consume less salt than potassium, at a ratio of about 4 to 1 in potassium’s favor (see Potassium).
Although conventional wisdom blames excess salt for high blood pressure and other problems, and most people on the Standard American Diet (SAD; note the pejorative expression) consume a lot of salt in their processed foods, it is still an essential mineral in physiology.
People have become sick and even died during long endurance contests by excessively diluting the salt content of their bodies with chronic excessive hydration (a condition known as hyponatremia). Even some of the best endurance athletes, marathoners, and long-distance triathletes have arrived at the finish line so depleted that they have to immediately receive an intravenous saline or sodium-chloride solution.
Along with potassium, salt is one of the important electrolytes of the body.
That said, it is easy to derive enough salt from whole nutritious foods (pastured eggs, high-quality cheeses, large salads, an electrolyte drink during a triathlon) without ever dusting your food with table salt.
Trace minerals are the minerals that we have to consume in our diet, drinking water, and/or a supplement in relatively small amounts. That’s not to say they are unimportant, though; see the upcoming sidebar on zinc and antinutrients, for example, or consider that iron represents the “heme” part of hemoglobin, our red blood cells that carry oxygen, and that selenium is a major antioxidant in the body.
Like the macrominerals, the microminerals include common elements that you will recognize from the periodic table (if you ever paid attention in Chemistry class). We’re just going to list the microminerals here, with helpful links for more details. The recommended levels for them range from around 10 milligrams to levels in the micrograms (1/1000 of a milligram, as in 55 mcg per day of selenium).
- Copper
The RDA for this mineral is 890 to 900 mcg per day (www.nlm.nih.gov/medlineplus/ency/article/002419.htm).
- Iodine
The RDA for this mineral is 150 mcg per day for adults (http://ods.od.nih.gov/factsheets/Iodine/).
- Iron
The RDA for this mineral is 8 mg per day for males and 18 mg/day for adult females (http://ods.od.nih.gov/factsheets/iron/).
- Manganese
The AI level for this mineral is 2.3 mg/day for adult males, and 1.8 mg for females (http://lpi.oregonstate.edu/infocenter/minerals/manganese/).
- Molybdenum
The RDA for this mineral is 45 mcg per day for adults (http://lpi.oregonstate.edu/infocenter/minerals/molybdenum/).
- Selenium
The RDA for selenium is 55 mcg for adults, 60 mcg for pregnant women, and 70 mcg for lactating moms (http://ods.od.nih.gov/factsheets/selenium/).
- Zinc
The RDA for zinc is 11 mg for adult males and 8 mg/day for females (http://ods.od.nih.gov/factsheets/Zinc-QuickFacts).
Okay, now you can take a deep breath. We’re finished with the vitamins/minerals, for the most part (but you shouldn’t be). Following is a description of various web tools that you can use to manage your micronutrients.
The Web is organic and abounds with new tools for analyzing diet, exercise, and other aspects of health. We’re going to discuss a couple of easy reference-oriented tools, meaning there’s little busy-work involved in jumping in and finding out what you need. You might want to keep up with the new apps, which have their own approaches and philosophies. Here’s a link tagged with “food” from Quantified Self: http://quantifiedself.com/guide/tag/food.
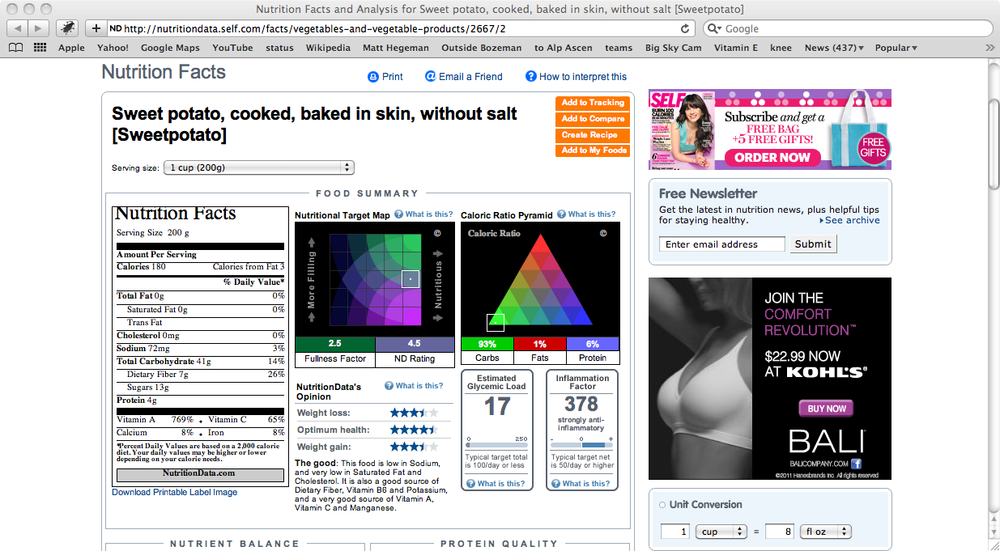
This indispensable tool is a user-friendly wrapper over the spartan but data-rich USDA National Nutrient Database (discussed momentarily, and in Chapter 2). Just search on any food, and you get a wealth of information on its protein, fat, and carbohydrate content (the macronutrients), along with very detailed information on micronutrients (vitamins and minerals). Figure 4-3 shows a browser window after a search on sweet potatoes.
Just scroll down to the Vitamins or Minerals segments of this page and click on the More Details widget, and you’ll likely discover many gems that you never knew before. For example, did you know that a large sweet potato contains about 1,922 micrograms of RAE for vitamin A? If you’ve already read the section on vitamin A, you know what an RAE is!
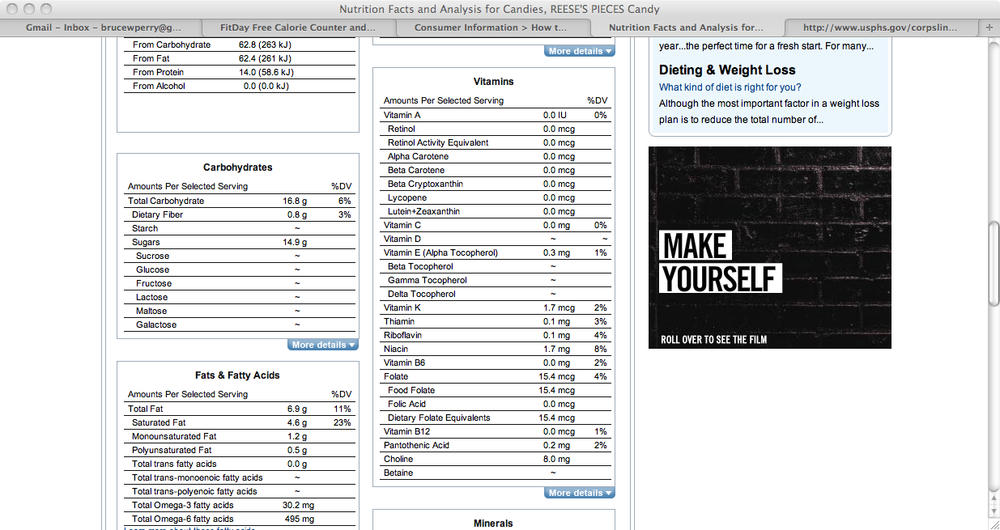
You can also reveal gaping holes in the nutrition department, as shown in Figure 4-4. This browser window shows the Vitamins frame of a NutritionData page after a search on Reese’s Pieces. Not much there, but there are almost 15 grams of simple sugar in a 1-ounce portion of the candy.
See Chapter 2 for more details on NutritionData.
Although presented as a weight-loss and dieting site, FitDay (www.fitday.com) is a very useful tool for entering your foods for the day and finding out the associated micronutrient content, or lack thereof.
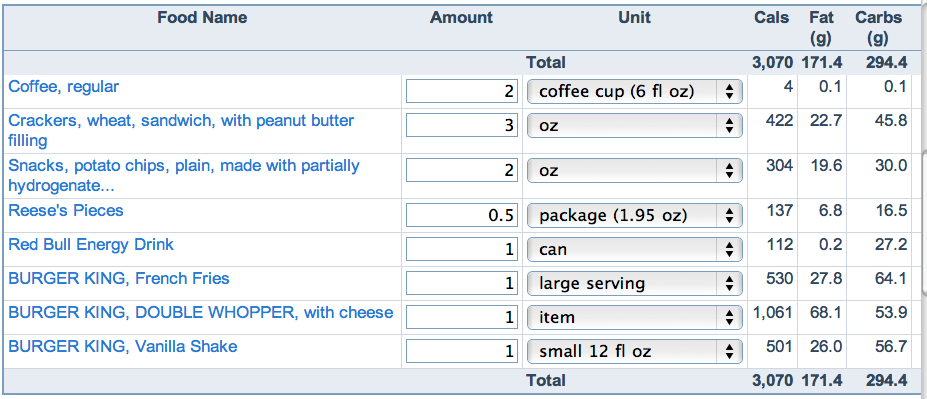
As a way of demonstrating how you can derive a vitamin and mineral profile for junk food—sorry, treats—from a vending machine and a fast-food joint, let’s enter these foods into FitDay and see what results the software displays.
Imagine you start off the day with a 12-ounce take-out coffee for breakfast; then later on you raid the vending machine for peanut butter crackers, some potato chips, and a package of Reese’s Pieces, which you mercifully leave only partially consumed. All this is washed down with a can of Red Bull. Finally, you top off the late afternoon by visiting the local fast food emporium and leaving with a Double Whopper and fries, with a vanilla shake in tow.
Figure 4-5 shows this fearsome lineup, as entered in FitDay.
Considering that only the bottom three items even remotely resemble an edible meal, one of the many data points that leaps off the page and begs for your attention is the calorie total: more than 3,000. The problem is that this chow-down represents a person’s consumption for only part of the day.
A mere 3 ounces of wheat crackers with peanut butter filling packs a pretty good wallop at 422 calories, considering that this snack is just a prelude for the heavy hitters that come afterward.
The table shows a lot of fat here, but it’s the type of fat that counts, as explained in Chapter 3. For example, the coconut milk that is part of a smoothie will tip the fat scale on FitDay, but this nutritious snack contains a portion of its fats in the form of lauric acid (which is a component of human breast milk).
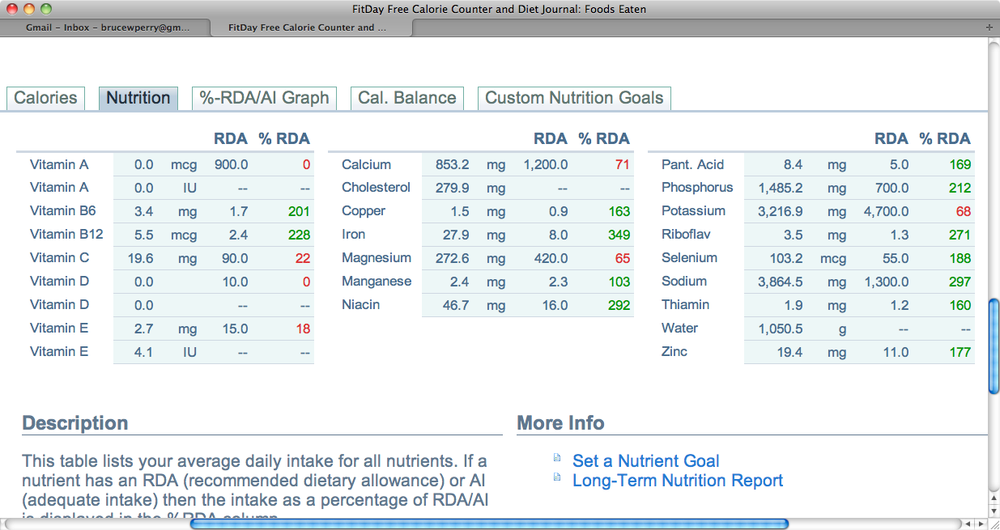
More of the bad to middling news comes on the Nutrition tab, which you can click on at the bottom of the page. Figure 4-6 shows this revealing table, indicating that the substances you gobbled up and guzzled down bore little resemblance to the food our forebears sustained themselves on.
The meal contains no vitamin A or D, and just enough C to perhaps prevent scurvy (but not for long). The table shows the RDA for each nutrient and the % RDA represented by the analyzed food. For example, the 201 adjacent to vitamin B6 indicates that the food contained about twice the recommended daily minimum amount of that nutrient. Deficits for a nutrient appear in red; it’s all pretty simple to read and understand.
Note
The good mineral profile here undoubtedly derives from the meat in the Double Whopper. This industrially mass-produced meat is far from a one-sided picture, however, as we saw in Chapter 3. For example, the meat probably came from a concentrated animal feeding operation (CAFO), and is not as healthy, to say the least, as meat from grazing animals that might be pastured near your town or city.
This motley collection of packaged chow contained just a fragment of the necessary vitamin E, which, along with the dearth of vitamin C, leaves you with few antioxidants to clean up after the day’s stresses (except for the selenium).
A diet like this will leave the body quivering and inflamed, given that the “fake” food contained almost zero phytochemicals with their associated antioxidants (see the Antioxidants: Cultivate Your Inner Nerf sidebar.) This means that some of the cellular damage, including of DNA, goes unchecked throughout the day.
The “meal” contained almost 1,200 calories’ worth of carbs, many of which were represented by simple sugars like sucrose and fructose, jacking up the inflammatory effects of an excess sugar load.
Another piece of data worth mentioning is the potassium to sodium ratio. Instead of the desirable ratio of about 4 to 1, this ratio was more like 0.84 to 1; in other words, the vending machine grazer is getting much more sodium than potassium, which has potentially dire effects down the road (see the Potassium section earlier in this chapter).
Of course, the point of this tongue-in-cheek exercise (no one really eats like this, right? Honest?) is to show FitDay’s useful, revealing, and sometimes sobering metrics when it comes to micronutrients. Once you get over the tedium of entering foods, the tool is fun to play with, and it gives you a precise enough micronutrient picture of your current food intake. It doesn’t deal with bioavailability (what quantities of these food nutrients actually make their way out of the gastrointestinal tract and to the body’s target tissues), so you can only use tables like these for general guidance.
See Chapter 2 for more details on FitDay.
The search widget at www.nal.usda.gov/fnic/foodcomp/search/ is the updated source of nutrition and food data that other tools, such as NutritionData (www.nutritiondata.com), use as an underlying data source. This database allows a simple search on terms like the name of a food or vitamin, as Figure 4-7 shows.
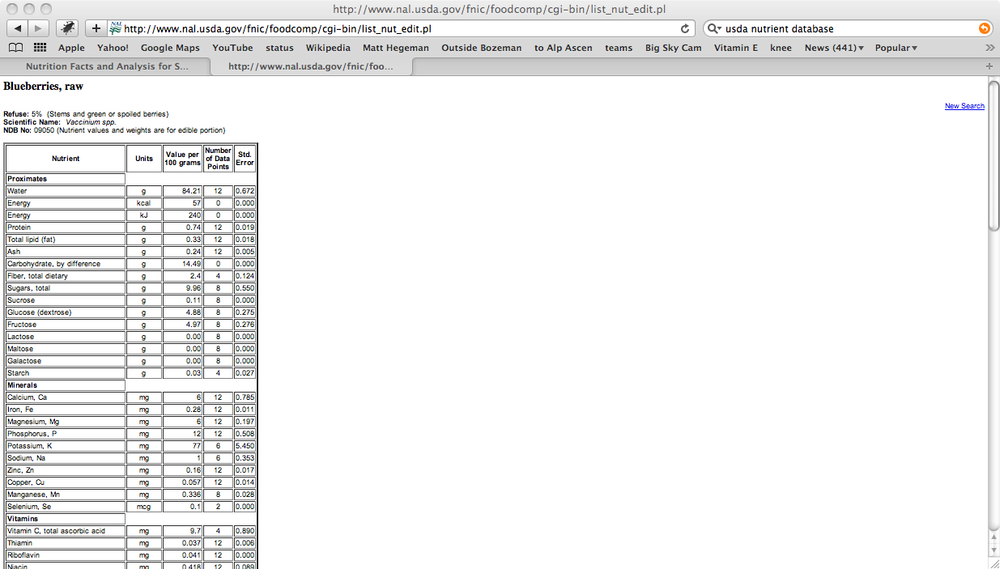
If you enter a certain food in the search space, the USDA nutrient database fires back a full page of data on that food’s nutrient content, including carbs, fats, protein, vitamins, and minerals. The information is presented in a simple HTML table but has impressive detail, as Figure 4-8 shows.
The USDA site also has a large archive of PDF reports on single nutrients: www.ars.usda.gov/Services/docs.htm?docid=20958. In addition, the entire database is downloadable itself. See Chapter 2 for more details on the USDA National Nutrient Database.
The LPI MIC (http://lpi.oregonstate.edu/infocenter/) has a wealth of useful information, including podcasts, comprehensive descriptions, and physiological background on individual micronutrients.
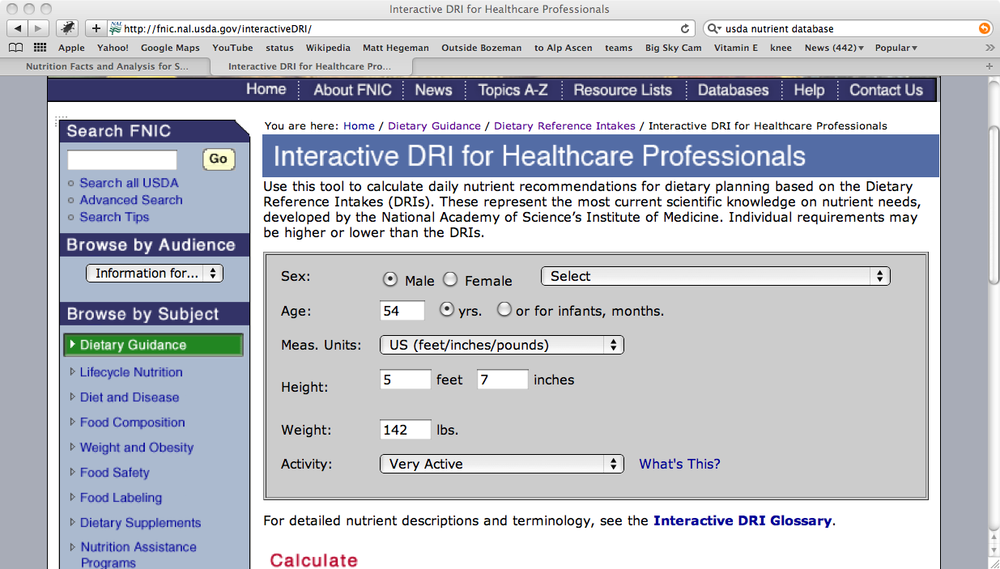
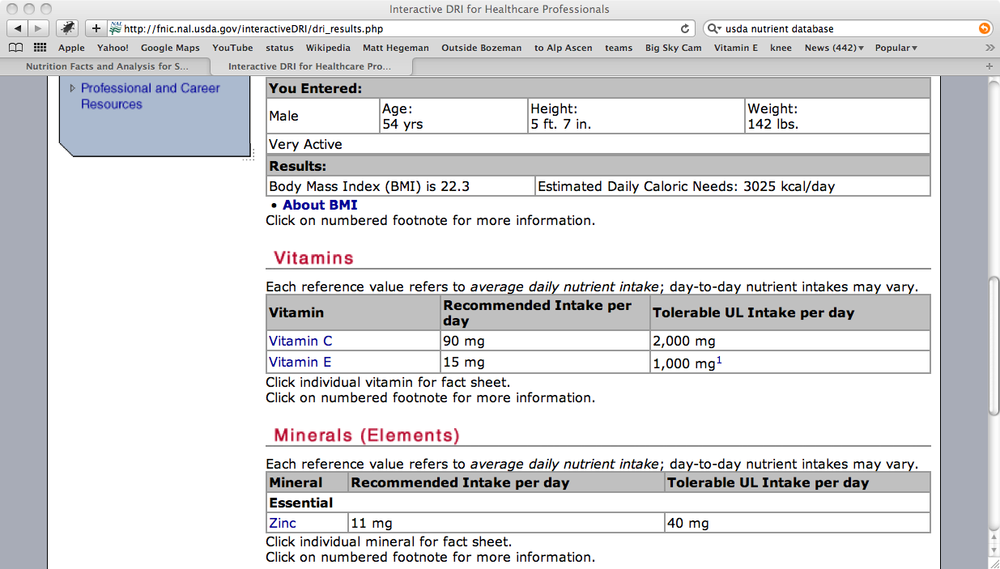
The USDA also has a handy calculator for estimating vitamin and mineral daily needs, based on your gender, height, and weight. Figure 4-9 shows the calculator’s front page, found at http://fnic.nal.usda.gov/interactiveDRI/.
As an example of just drilling down to a few data points, I wanted to look at my own requirements for vitamins C and E, as well as for the mineral zinc. Figure 4-10 shows the result. This is a very good little calculator for checking the mineral content of an MVM supplement, for example.
Although still incomplete (they only cover, for the most part, vitamins), the NIH factsheets at http://ods.od.nih.gov/factsheets/list-all/ contain all the necessary data on these micronutrients, including food sources, RDAs, and TULs.
Get Fitness for Geeks now with the O’Reilly learning platform.
O’Reilly members experience books, live events, courses curated by job role, and more from O’Reilly and nearly 200 top publishers.